Cranial Nerves
👩⚕️ This lesson is long but extremely high–yield. Learn the lesion patterns, muscle actions, and skull foramina cold.
3️⃣ Oculomotor CN III
- The oculomotor nerve supplies medial rectus, superior rectus, inferior rectus, inferior oblique, and levator palpebrae superioris.
- It also carries parasympathetic fibres via the ciliary ganglion to the sphincter pupillae.
Features of CN III palsy
- [[Down-and-out eye::Down-and-out eye due to paralysis of the medial rectus]]
- [[Ptosis::Ptosis due to paralysis of the levator palpebrae superioris]]
- [[Mydriasis::Remember that the oculomotor CN III facilitates pupil constriction via its parasympathetic innervation to the sphincter pupillae through the ciliary ganglion]]
Causes of CN III nerve palsy:
- False localising sign due to uncal herniation in high ICP due to an expanding extradural haematoma
- + headache = Posterior communicating artery aneurysm
- + contralateral hemiplegia = Weber’s syndrome
- Medical: Amyloid, multiple sclerosis, temporal arteritis, SLE, diabetes
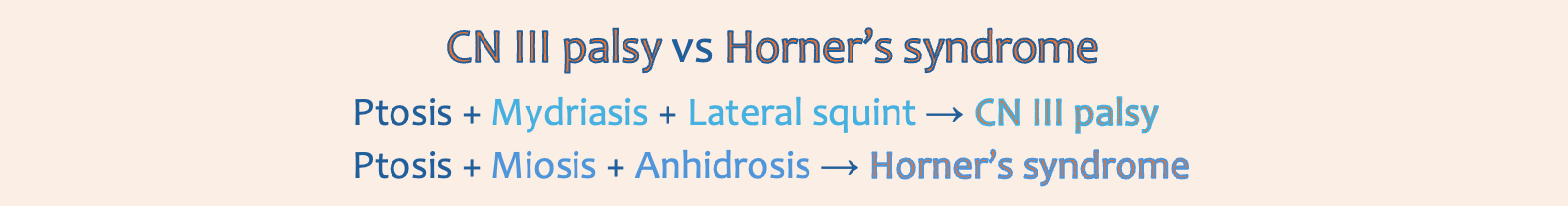
👁️ In Oculomotor CN III palsy, severe ptosis occurs due to loss of motor innervation to the levator palpebrae superioris, skeletal muscle that lifts the eyelids.
👁️ In Horner’s syndrome, mild ptosis occurs due to loss of sympathetic innervation to the superior tarsal muscle, smooth muscle that helps hold the eyelids elevated.
A patient develops a down-and-out-eye after neck surgery. Which accompanying feature is likely?
- ((Exophthalmos::Typical of Graves’ orbitopathy due to inflammatory enlargement of extraocular muscles and orbital fat, not from an isolated oculomotor CN III palsy.))
- [[Mydriasis::CN III carries parasympathetic fibres to the sphincter pupillae via the ciliary ganglion; damage prevents constriction and produces an ipsilateral dilated pupil.]]
- ((Nystagmus::Usually reflects vestibular or cerebellar pathology involving the vestibulocochlear CN VIII, not selective medial rectus and levator palpebrae weakness.))
- ((Loss of corneal reflex::Corneal reflex depends on V1 (sensory) and VII (motor to orbicularis oculi); CN III palsy does not abolish it.))
A patient sustains head trauma and presents to A&E conscious. He is noted to have a right, fixed and dilated pupil. A few hours later, he deteriorates and dies. What is the likely cause?
- ((Left extradural haematoma::A left-sided extradural would compress the left oculomotor nerve, producing a left dilated pupil, not right-sided pupillary dilation.))
- [[Right extradural haematoma::A right temporal extradural can cause uncal herniation, compressing the right oculomotor nerve → ipsilateral fixed dilated pupil followed by rapid deterioration.]]
- ((Acute subdural haematoma::Tearing of the bridging veins leads to a more gradual decline))
- ((Subarachnoid haemorrhage::Presents with thunderclap headache and meningism))
4️⃣ Trochlear CN IV
Trochlear CN IV innervates the superior oblique, responsible for depressing the adducted eye. Injury classically leads to difficulty reading or descending stairs.
A man with diplopia is unable to look down and inwards with his right eye. Which nerve is affected?
- ((Abducens nerve::Controls lateral rectus, abducts the eye))
- ((Ciliary ganglion::Parasympathetic oculomotor CN III fibres for pupil constriction and lens accommodation))
- ((Nasociliary nerve::Sensory branch of CN V1, no motor function))
- [[Trochlear nerve::Supplies superior oblique for depression of the adducted eye]]
5️⃣ Trigeminal CN V
👩⚕️ Separate lesson for this one...
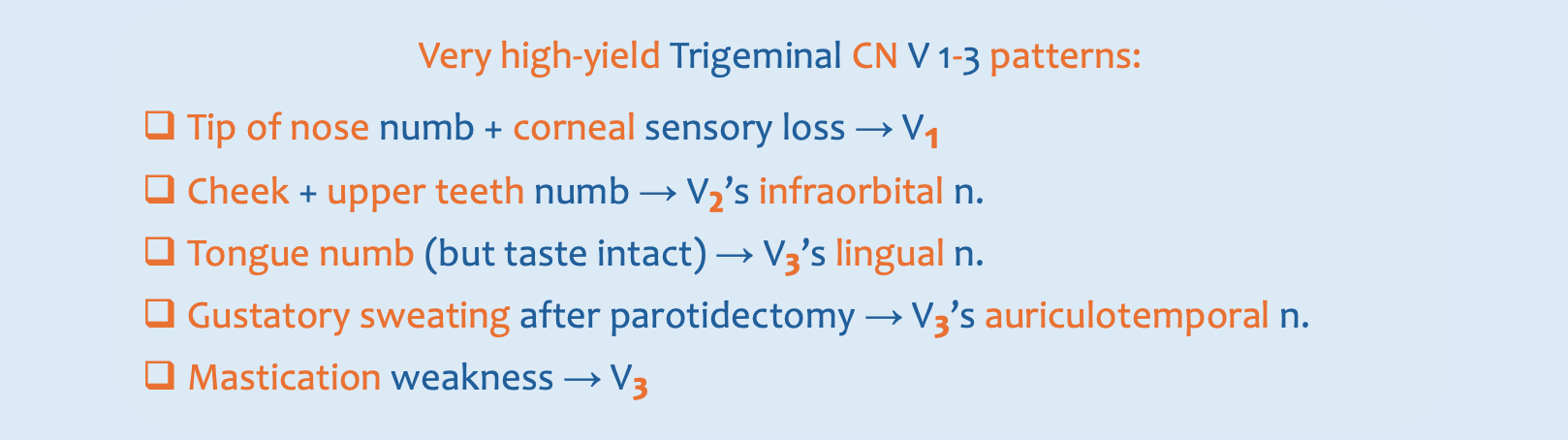
A 22‑year‑old woman has lost sensation over the tip of her nose. Where else is sensation likely to be lost?
- ((Hard palate::Sensation via the greater palatine branch of trigeminal’s maxillary CN V2))
- ((Soft palate::Sensation via the lesser palatine branch of trigeminal’s maxillary CN V2 and glossopharyngeal CN IX))
- ((Ear pinna::Supplied by multiple nerves including greater auricular, lesser occipital and auriculotemporal nerves))
- [[Cornea::CN V1 branches include the external nasal nerve off the anterior ethmoidal n. which supplies the nasal tip, and the nasociliary nerve which provides sensation from the cornea via the ciliary ganglion.]]
A patient presents with numbness of the cheek, upper frontal teeth, and anesthesia of the lateral side of the nose following facial trauma. Which nerve is most likely injured?
- [[Infraorbital::Terminal branch of maxillary V₂; supplies the cheek, upper lip, lateral nose, and upper incisors—classically injured in orbital floor and zygomatic fractures.]]
- ((Infratrochlear::Branch of the nasociliary from CN V₁; supplies the medial canthus and bridge of the nose.))
- ((Supratrochlear::Branch of the frontal nerve from CN V₁; supplies the medial forehead and upper eyelid.))
- ((Anterior superior alveolar::Branch of infraorbital; supplies upper incisors.))
The infraorbital nerve, the terminal branch of the trigeminal’s maxillary CN V2, exits via the infraorbital foramen. It may be injured in zygomatic or orbital floor fractures, causing numbness of the lower eyelid, cheek, lateral nose, upper lip, upper incisors and canines.
Within the infraorbital canal, the infraorbital nerve gives off the middle and anterior superior alveolar nerves. Emerging from the infraorbital canal, it gives off the inferior palpebral, nasal and superior labral branches.
6️⃣ Abducens CN VI
7️⃣ Facial CN VII
👩⚕️ Separate lesson for this one also!
A 21-year-old man undergoes surgical removal of an impacted third molar. Post-operatively, he has anaesthesia of the anterolateral tongue. What nerve was most likely injured?
- Marginal mandibular branch::of CN VII: Motor to lower limb and chin
- Hypoglossal CN XII::Motor to 7 of 8 tongue muscles
- Glossopharyngeal CN IX::General and taste sensation from posterior ⅓ of tongue, sensory from middle ear
- Inferior alveolar::of CN V3: Sensation from lower teeth, lower gum, lower lip and chin
- Lingual::✔
- The lingual nerve from trigeminal’s mandibular CN V3 provides general sensation to the anterior ⅔ of the tongue
- The chorda tympani from facial CN VII provides taste to the anterior ⅔ of the tongue
- The glossopharyngeal CN IX provides general sensation & taste to posterior ⅓ of tongue
- The hypoglossal CN XII provides motor supply to 7 of 8 tongue muscles
- The vagus CN X provides motor supply to the palatoglossus
- A 23-year-old woman with sialolithiasis of the submandibular gland is undergoing surgical excision. During mobilisation of the submandibular duct, which nerve is most at risk?
- Lingual::✔
The lingual nerve is medial to the 3rd molar and near to the submandibular duct, so it’s highly vulnerable during lower 3rd molar extraction and submandibular duct mobilisation or removal.
- During a parotidectomy, transection of the facial nerve is a risk. Which would not result from facial nerve injury?
- Numbness over the cheek::✔Sensory: Buccal n. from trigeminal’s mandibular CN V3
- Loss of corneal reflex::Orbicularis oculi is supplied by the zygomatic and temporal b. of facial CN VII
- Lower lip dropping::Depressor labii inferioris is supplied by the marginal mandibular b. of facial CN VII
- Drop angle of mouth::Depressor anguli oris supplied by buccal and marginal mandibular b. of facial CN VII
- A patient has a facial nerve injury following left parotid surgery. Which of these abnormalities is most likely?
- Ptosis of the left eyelid::Levator palpebrae superioris, innervated by oculomotor CN III
- Drooping of the left lower lip::✔
- Numbness on the whole face::Trigeminal CN V
- Numbness of the ipsilateral cheek::Buccal b. of the trigeminal’s trigeminal’s mandibular CN V3
- A patient developed an uneven smile after an upper deep cervical lymph node biopsy. Which nerve was most likely injured?
- Buccal
- Mental
- Inferior alveolar branch
- Marginal mandibular branch::✔Motor to muscles of lower lip (depressor anguli oris)
The marginal mandibular branch of the facial CN VII innervates the muscles of the lower lip e.g. depressor anguli oris, depressor labii inferioris, and mentalis. It runs along the lower border of the mandible, and is very superficial, making it highly susceptible to injury during surgery involving the parotid gland or submandibular area. Injury results in drooping of the lower lip on smiling or talking on the affected side.
- A patient develops gustatory sweating following a parotidectomy. What is the mechanism behind this condition?
- Regeneration of the parasympathetic fibres of auriculotemporal nerve innervating the sweat gland::✔
- Regeneration of sympathetic fibres on the parasympathetic of auriculotemporal nerve
- Regeneration of facial nerve after its injury
- Regeneration of great auricular nerve on sympathetic fibres innervating the sweat gland
The auriculotemporal nerve is a branch of the mandibular CN V3, which has three functions:
- Sensory from temple, TMJ, external acoustic meatus, anterior to auricle, tragus, crus
- Parasympathetic fibres to the parotid gland for saliva production
- The auriculotemporal nerve (of the mandibular CN V3) receives postganglionic parasympathetic fibres from the lesser petrosal nerve from the otic ganglion, derived from the glossopharyngeal CN IX.
- Sympathetic fibres to the sweat glands and blood vessels of the skin
Frey’s syndrome (gustatory sweating) happens when the auriculotemporal nerve is damaged e.g. during parotid surgery. As the nerve heals, the parasympathetic fibres regrow along the wrong pathway into the sweat glands and blood vessels of the skin instead of growing to the parotid gland. As a result, when the patient eats and the body tries to stimulate salivation, it instead triggers sweating and flushing over the area near the parotid.
The middle meningeal artery is closely related to the auriculotemporal nerve; the nerve actually wraps around the artery, making both structures easy to identify in anatomy dissections but also vulnerable during surgery.
A 58-year-old suffering from a tumor invading the base of the cavernous sinus. Which nerve is involved?
- ((Mandibular V3::Exits the skull via the foramen ovale along with the accessory meningeal artery and lesser petrosal nerve.))
- [[Abducens CN VI::Runs through the center of the cavernous sinus adjacent to the internal carotid artery.]]
- ((Facial CN VII::Leaves the skull through the stylomastoid foramen after passing through the facial canal.))
- ((Vestibulocochlear CN VIII::Travels with the facial nerve through the internal acoustic meatus.))
- ((Glossopharyngeal CN IX::Exits via the jugular foramen along with the vagus and accessory nerves.))
Which nerve passes centrally through the cavernous sinus?
Abducens CN VI
In a case of cavernous sinus thrombosis, which of the following nerves is most likely to be injured, especially considering that it lies within the sinus rather than in its lateral wall?
- ((Optic nerve::Travels through the optic canal accompanied by the ophthalmic artery.))
- ((Oculomotor nerve::Runs in the lateral wall of the cavernous sinus alongside the trochlear and ophthalmic nerves.))
- [[Abducens nerve::Passes centrally through the cavernous sinus next to the internal carotid artery, making it highly vulnerable to thrombosis.]]
- ((Ophthalmic nerve V1::Courses within the lateral wall of the cavernous sinus with oculomotor and trochlear nerves.))
The abducens CN VI is the first to suffer injury in sinus thrombosis or compression by tumors at its base, presenting as lateral rectus palsy with an inability to abduct the eye; the affected eye will turn inward, leading to horizontal double vision particularly when looking to the side of the affected eye. When venous drainage from the orbit is obstructed due to cavernous sinus thrombosis, it leads to: Oedema of the conjunctiva and eyelids, exophthalmos, transmitted pulsations from the internal carotid artery, and ophthalmoplegia with abducens palsy. On ophthalmoscopy, there is evidence of papilloedema and retinal haemorrhages.
Structures that travel through the cavernous sinus:
- Abducens CN VI
- Carotid plexus
- Internal carotid artery
Structures that travel through the lateral wall of the cavernous sinus:
- Oculomotor CN III
- Trochlear CN IV
- Trigeminal's Ophthalmic CN V1 branches
- Trigeminal's Maxillary CN V2 branches
- A 45‑year‑old woman 10 months post‑parotidectomy presents with facial palsy. Which feature is expected?
- Dropping of angle of mouth::✔Injury to the marginal mandible branch of CN VII leads to lower face droop
- Loss of sensation to angle of jaw::Great auricular nerve
- Scalp loss of sensation::Great auricular or trigeminal
- Weakness of muscles of mastication::Trigeminal’s mandibular CN V3
It is useful to understand the anatomical course of the facial CN VII to understand how lesions at different sites may manifest. The first part of the course is intracranial:
- The facial CN VII’s two roots (a large motor and small sensory root) arise from the pons, travel through the internal acoustic meatus of the temporal bone, and enter the Z-shaped facial canal. In the facial canal the two roots fuse to form the facial CN VII which then forms the geniculate ganglion.
- The nerve gives rise to the following three branches:
- Greater petrosal nerve
- Nerve to stapedius
- Chorda tympani
- It gives these off then exits the facial canal and exits the cranium via the stylomastoid foramen which marks the start of its extracranial course. On exiting the skull, the facial nerve runs just anterior to the outer ear and the first extracranial branches to arise are the:
- Posterior auricular nerve
- Posterior belly of the digastric muscle motor branch
- Stylohyoid motor branch
- The remaining main trunk, the motor root of the facial nerve, continues anteriorly and inferiorly into the parotid gland within which it terminates by splitting into five branches:
- Temporal branch
- Zygomatic branch
- Buccal branch
- Marginal mandibular branch
- Cervical branch
- The chorda tympani exits through which foramen?
- Petrotympanic fissure::✔Travels from the facial canal, through the middle ear, out via the petrotympanic fissure
- Which of the following is the cause of hyperacusis?
- Nerve to stapedius::✔The nerve to stapedius, a branch of CN VII, dampens sound; damage causes hyperacusis
- A 50-year-old man fell at work and was unconscious for several minutes. In the ED, he complains only of hyperacusis. Which nerve is most likely injured?
- Facial::✔The nerve to stapedius, a branch of CN VII, dampens sound; damage causes hyperacusis
- A man with a skull injury develops ipsilateral facial muscle weakness, but no hyperacusis or taste disturbance. Where is the most likely site of facial nerve injury?
- Stylomastoid foramen::✔At this point the nerve has exited the skull, only motor branches to facial muscles remain
Injury to the internal acoustic meatus or middle ear would involve chorda tympani (loss of taste) and nerve to stapedius (hyperacusis). Injury at the parotid gland would affect specific branches variably, not cause total unilateral weakness. This presentation suggests a lesion after the nerve to stapedius and chorda tympani have branched off, at the stylomastoid foramen, resulting in pure motor facial paralysis.
- A patient suffers an orbital floor fracture and now has loss of lacrimation. Which nerve is most likely affected?
- Lacrimal::Sensory only
- Facial::Would cause broader facial paralysis
- Greater petrosal::✔Carries parasympathetic fibres to lacrimal gland
- Auriculotemporal::Parasympathetic to parotid, not lacrimal
Lacrimation reflex pathway: Conjunctiva irritation → Lacrimal n. → Ophthalmic n. (V1) → Trigeminal sensory centre → Superior salivary nucleus → Facial CN VII → Greater petrosal n. → Pterygopalatine ganglion → Joins zygomatic branch of trigeminal’s maxillary CN V2 → Joins the lacrimal branch of V1 → Lacrimal apparatus
Arterial supply to the lacrimal system is via a lacrimal branch of the ophthalmic artery of the internal carotid artery.
Venous drainage is to the superior ophthalmic vein.
- A patient presents with loss of lacrimation. Which ganglion is involved?
- Otic::Via CN IX to the parotid gland
- Submandibular::CN VII to the submandibular and sublingual glands for salivary secretion
- Pterygopalatine::✔Parasympathetic relay for lacrimal gland
- Ciliary::Parasympathetic fibres from VN III, for pupil constriction and accommodation
- A patient underwent parotidectomy followed by radiation therapy, and later presents with dryness of the eyes. Which ganglion is most likely involved?
- Pterygopalatine::✔
- Otic::Joins parasympathetic CN IX fibres with Auriculotemporal b. Of CN V3 to the parotid gland
- Ciliary::Parasympathetic fibres from CN III, for pupil constriction and accommodation
- Submandibular::CN VII to the submandibular and sublingual glands for salivary secretion
- Four parasympathetic ganglia in the head and neck
- Ciliary ganglion to the ciliary and pupillae sphincter muscles
- Pterygopalatine (aka sphenopalatine) ganglion to the lacrimal glands
- Submandibular ganglion to the submandibular and sublingual glands
- Otic ganglion to the parotid glands
- Edinger-Westphal nucleus → Oculomotor CN III → Ciliary ganglion → Short ciliary nerves → Pupillary sphincter and ciliary muscles
- Superior salivary nucleus → Facial CN VII → Greater petrosal n. → Pterygopalatine ganglion → Joins zygomatic branch of trigeminal’s maxillary CN V2 → Joins the lacrimal branch of V1 → Lacrimal apparatus
- Superior salivary nucleus → Facial CN VII → Internal acoustic meatus → gives off the Chorda tympani → Joins the lingual nerve of trigeminal’s mandibular CN V3 → Submandibular ganglion → Parasympathetic supply to submandibular and sublingual glands
- Inferior salivatory nucleus → Glossopharyngeal CN IX → Tympanic n. of Jacobson → Passes through the jugular foramen and enters the middle ear to form the tympanic plexus → Lesser petrosal n. → Exit the skull through the foramen ovale → Otic ganglion → Joins the auriculotemporal branch of V3 → Parotid gland
- An elderly lady with sensorineural hearing loss has a cerebellopontine angle lesion. What nerve is likely affected?
- Vestibulocochlear::✔CN VIII; responsible for hearing and balance
- A healthy 55-year-old woman presents with left-sided high-frequency hearing loss and dizziness. Normal external and middle ear exam. What is the most likely cause?
- Dermoid cyst::Not common in the internal auditory canal
- Cholesteatoma::Conductive hearing loss, chronic foul smelling ear discharge, facial nerve palsy
- Malignant otitis externa::Severe otalgia, facial nerve palsy in a diabetic, due to pseudomonas aeruginosa
- Paraganglioma::Causes pulsatile tinnitus
- Schwannoma::✔Sensorineural hearing loss, vertigo
Progressive sensorineural hearing loss indicates vestibular schwannomas (acoustic neuromas) arising from vestibulocochlear CN VIII at the cerebellopontine angle, often high-frequency first, and vertigo with balance issues.
Cranial nerves IV to XI pass near or within the cerebellopontine angle. The commonest lesion to affect this site is an acoustic neuroma most commonly compromising the vestibulocochlear CN VIII. Larger lesions may affect the facial CN VII which lies closest to this site, and the trigeminal CN V, presenting with ipsilateral loss of corneal reflex and hearing.
- Damage to both the vagus CN X and hypoglossal CN XII would occur at which level of the central nervous system?
- Medulla::✔Nuclei for CN IX, X, XI and XXI are in the medulla oblongata
- Nuclei for CN III and IV are in the midbrain.
- Nuclei for CN V, VI, VII and VIII are in the pons.
- Nuclei for IX, X, XI and XXI are in the medulla oblongata.
- A patient presents with loss of sensation over the tongue and soft palate. Which brainstem region is affected?
- Medulla::✔
- Sensation of posterior ⅓ of tongue and soft palate is via Glossopharyngeal CN IX, which arises from the medulla. Pons (CN V) only supplies anterior ⅔ of tongue (general sensation) and facial dermatomes.
Vagus CN X
A man has hoarseness following neck surgery. Which cranial nerve does the responsible nerve branch from?
- [[Vagus CN X::The recurrent laryngeal nerve, which supplies the vocal cords, branches from the vagus nerve and its injury leads to hoarseness.]]
- ((Glossopharyngeal CN IX::The glossopharyngeal nerve provides sensory supply to the oropharynx and taste to the posterior third of the tongue.))
- ((Accessory CN XI::The accessory nerve supplies the sternocleidomastoid and trapezius muscles.))
- ((Hypoglossal CN XII::The hypoglossal nerve provides motor supply to the intrinsic and extrinsic muscles of the tongue.))
Carotid endarterectomy
Carotid endarterectomy involves dissecting the sternocleidomastoid muscle, ligating of the common facial vein and then dissecting the internal jugular to expose the common and the internal carotid arteries. Nerves at risk during this:
- ((Hypoglossal CN XII:: Provides motor innervation to ⅞ of tongue muscles so injury causes tongue deviation))
- ((Greater auricular nerve::Provides sensation from angle of mandible and parotid region))
- ((Superior laryngeal nerve::Enables pitch modulation, so injury affects the pitch of voice))
- ((Recurrent laryngeal nerve::Provides motor innervation to vocal cords, so injury causes hoarseness))
Carotid sheath
- Contents of the carotid sheath:
- Medially: Common carotid artery, which divides into the external and internal carotid artery
- Posteriorly: Vagus CN X
- Laterally: Internal jugular vein
- Anteriorly: The carotid sheath is crossed anteriorly by the hypoglossal CN XII and the ansa cervicalis.
- Posteriorly: The cervical sympathetic chain lies posteriorly between the sheath and the prevertebral fascia.
Which of the structures listed below is a content of the carotid sheath?
- ((External jugular vein::The external jugular vein runs superficial to the sternocleidomastoid muscle.))
- ((Phrenic nerve::The phrenic nerve runs on the anterior surface of the anterior scalene muscle.))
- ((Hypoglossal CN XII::The hypoglossal nerve crosses the carotid arteries after exiting the hypoglossal canal.))
- ((Recurrent laryngeal nerve::The recurrent laryngeal nerve travels in the tracheoesophageal groove.))
- [[Vagus CN X::The vagus nerve runs between the internal jugular vein and the common carotid artery within the carotid sheath.]]
Accessory CN XI
During a Level V neck dissection in the posterior triangle, which nerve is most at risk of injury?
Spinal accessory CN XI
The spinal accessory CN XI crosses the posterior triangle, running superficially and is highly vulnerable during lymph node biopsies or neck dissections. Injury can lead to trapezius muscle weakness, resulting in shoulder droop and difficulty in > 90° shoulder abduction. It is one of the most common iatrogenic nerve injuries in the neck.
Which neck triangle?:💥 X: anterior, XI: posterior, XII: anterior
During a Level V neck dissection in the posterior triangle, which nerve is most at risk of injury?
- [[Spinal accessory nerve::The spinal accessory nerve crosses superficially through the posterior triangle and supplies the trapezius, making it highly vulnerable during Level V dissections.]]
- ((Phrenic nerve::The phrenic nerve runs on the anterior surface of the anterior scalene muscle and provides motor supply to the diaphragm.))
- ((Long thoracic nerve::The long thoracic nerve descends along the lateral chest wall and supplies the serratus anterior muscle.))
- ((Dorsal scapular nerve::The dorsal scapular nerve arises from the brachial plexus and supplies the rhomboids and levator scapulae muscles.))