Lower Limb

Acetabular Labral Tears
MRI, ideally with intra‑articular contrast (MR arthrogram), is the gold standard to detect acetabular labral tears.
A patient with suspected acetabular labral tear needs the best imaging. Which investigation is most appropriate?
MRI
Lateral cutaneous nerve of the thigh
Lateral cutaneous nerve of the thigh is a direct branch of the lumbar plexus at L2, L3 and emerges on the lateral border of the psoas muscle. Paraesthesia over the lateral thigh elicited by tapping the inguinal ligament suggests entrapment or irritation of the lateral cutaneous nerve beneath the inguinal ligament, a condition known as meralgia paresthetica.
During surgery, the surgeon caused damage to the nerve near the lateral border of psoas major. The patient experienced numbness over the lateral thigh. Which nerve was affected?
Lateral cutaneous nerve of thigh
What is the nerve root origin of the lateral cutaneous nerve of the thigh?
L2 and L3
A man has paraesthesia over the lateral aspect of his left thigh elicited by tapping on the inguinal ligament. What is the root of the causative nerve?
L2 and L3
The lateral cutaneous nerve is formed by fibres from roots _ _ and emerges on the _ border of the _ muscle.
The lateral cutaneous nerve is formed by fibres from L2 and L3 and emerges on the lateral border of the psoas muscle.
A 44-year-old man with HIV has a large abscess along the lateral border of psoas major muscle causing pressure on the nerves that exit the muscle in this region. Which of the following features is likely to be found?
- ((Loss of sensation on the lateral aspect of the lower leg::Sciatic nerve))
- [[Meralgia paresthetica::Meralgia paresthetica describes paraesthesia over the lateral thigh elicited by tapping the inguinal ligament suggests entrapment or irritation of the lateral cutaneous nerve beneath the inguinal ligament.]]
- ((Loss of sensation on the sole of the foot::Tibial nerve))
- ((Weakness of hip abduction::Superior gluteal nerve))
- ((Weakness of hip adduction::Obturator nerve))
Femoral nerve
The femoral nerve (L2, L3, L4) supplies anterior thigh sensation via the anterior cutaneous branches, and the quadriceps muscle for knee extension. It may be injured during lower abdominal surgery like hernia repair.
A patient suffered a sensory deficit over the anterior thigh with an inability to extend the knee after an open hernia repair. What is the affected nerve?
Femoral nerve
A patient developed sensory loss over his left knee and medial aspect of the leg. Which nerve root is affected?
L4
Saphenous nerve
The saphenous nerve, a terminal purely sensory branch of the femoral nerve, originates from L3,L4, and provides cutaneous sensation to the medial aspect of the leg, ankle and foot. It is vulnerable in thigh/leg surgery.
A woman develops sensory loss over the medial aspect of her leg after varicose vein surgery. Which nerve is most likely injured?
- ((Deep peroneal nerve::Supplies the first dorsal web space))
- ((Sural nerve::Supplies lateral foot/ankle))
- [[Saphenous nerve::Saphenous nerve is a purely sensory branch of the femoral nerve to the medial leg]]
- ((Superficial peroneal nerve::Anteriolateral aspect of leg))
- ((Tibial nerve::Sole and plantar foot))
A patient with back pain develops lateral foot numbness, with weakness in dorsiflexion of the ankle and hallux. The ankle and knee jerk reflexes are intact. What nerve root is the cause?
- [[L5::Lesion of L5 causes weakness of ankle and hallux dorsiflexion, sensory loss over the lateral leg and dorsum of the foot, while ankle (S1) and knee (L3,L4) reflexes remain normal.]]
- ((L4::L4 lesions cause impaired knee extension and reduced knee jerk reflex, with sensory loss over the medial leg.))
- ((S1::S1 lesions cause loss of plantarflexion, loss of the ankle jerk reflex, and sensory loss over the posterior calf and sole.))
- ((S2::S2 lesions typically affect posterior thigh/leg sensation and sphincter function.))
A 45-year-old man presented with backache and leg pain due to a prolapsed lumbar intervertebral disc. The pain, which is aggravated by coughing and sneezing, radiates to the dorsum of the foot. On examination there is weakness of the dorsiflexion of the foot. Which nerve root is most likely to be involved?
L5
A patient with dorsal foot pain is found to have a disc prolapse with loss of toe extension, and reduced ankle dorsiflexion with foot drop and a high stepping gait. Which is the likely involved root?
L5
A patient with dorsal foot pain is found to have a disc prolapse with loss of toe extension, and reduced ankle dorsiflexion with foot drop and a high stepping gait. Which is the likely involved root?
L5
A man presents with back pain and leg pain due to a prolapsed lumbar intervertebral disc. Examination shows weakness of both extensor digitorum and extensor hallucis longus. What is the most likely root lesion?
L5
A patient presents with difficulty in lifting the front part of the foot while walking and frequently trips over the toes. There is weakness of ankle dorsiflexion. Which myotome is primarily responsible for this movement?
A patient presents with difficulty lifting the front part of the foot while walking and frequently trips over the toes. There is weakness of ankle dorsiflexion. Which myotome is primarily responsible for this movement?
- [[L4, L5::These roots supply the deep peroneal nerve, which innervates tibialis anterior — the main dorsiflexor of the ankle. Weakness classically indicates L4/L5 involvement.]]
- ((L3::Primarily supplies hip flexion and knee extension))
- ((S1::Controls plantarflexion (via gastrocnemius/soleus) and the ankle jerk reflex))
- ((S2::Contributes to intrinsic foot muscles and plantarflexion))
A 55-year-old man presents with acute back pain. Neurological examination reveals both lack of sensation and weakened dorsiflexion of the left great toe. Which spinal nerve of the left side has been affected?
L5
L5 supplies dorsiflexion, toe extension, and sensation over the lateral leg and dorsum of the foot. Reflexes are spared, which helps distinguish L5 from L4 or S1 lesions: S1 contributes to the Achilles reflex, and L3 and L4 the Patellar reflex.
Functions of the L5 nerve root
- L5 innervates extensor hallucis longus (via the deep peroneal nerve), allowing big toe extension
- L5 innervates tibialis anterior muscle (via the deep peroneal nerve), allowing ankle dorsiflexion
- L5 supplies sensation to the the lateral leg and dorsum of the foot, including the hallux
- L5::✔
What is the spinal root value of the tibial nerve?
- L4 to S3::✔The tibial nerve is the larger terminal branch of the sciatic nerve, originating from L4 to S3.
- A man has backache and leg pain due to a prolapsed lumbar intervertebral disc. The pain is aggravated by coughing and sneezing, and radiates to the lateral aspect of the foot. There is weakness of the plantarflexors of the foot. Which nerve root is most likely involved?
- S1::✔
Functions of the S1 nerve root
- Innervates the gastrocnemius and soleus, via the tibial nerve, allowing plantarflexion
- Sensation to the posterolateral leg and lateral foot, via the sural nerve, which arises from the joining of terminal branches of the tibial and common peroneal nerve
- Achilles reflex, via S1 and S2 (tie your shoe) of the tibial nerve
- A 50-year-old under medical treatment of systemic lupus erythematosus presents to A&E after a fall. An X-ray shows a displaced subcapital femoral neck fracture with an area of radiolucency in the femoral head. The patient undergoes hemiarthroplasty. Which medication for SLE is the most likely cause for her presentation?
- Prednisolone::✔Long-term corticosteroids are the most common drug-related cause of avascular necrosis
- A man is brought to the resuscitation room following a motorcycle accident. On examination, his right thigh is found to be swollen and tense. His right foot is pale and cold and legs in external rotation. Diagnosis?
- Anterior dislocation of the hip::Causes shortened, externally rotated leg, not thigh swelling
- Central fracture dislocation of the hip::More common in side-impact injuries
- Fractured neck of femur::Not associated with tense thigh swelling
- Fractured shaft of femur::✔Fits trauma mechanism, tense swelling, pale foot
A fractured femoral shaft can cause significant bleeding, swelling, and vascular compromise, especially in high-energy trauma. Prompt assessment for compartment syndrome is key.
- A 53‑year‑old male suffers trauma to his left thigh. He has thigh tenderness on external rotation, a large thigh swelling, and absent distal pulses. What is the most likely cause?
- Femoral shaft fracture::✔Thigh deformity, thigh swelling, vascular (femoral a.) compromise, absent pulses
- Anterior hip dislocation::Hip flexed and abducted
- Posterior hip dislocation::Internally rotated hip, risk sciatic nerve
- Slipped femoral epiphysis::Adolescent, not acute trauma
- An athlete suffered an RTA resulting in a medially rotated thigh with a large swelling at the midthigh. Diagnosis?
- Neck of femur fracture
- Posterior hip dislocation with sciatic nerve injury
- Anterior hip dislocation
- Femur shaft fracture::✔
- A patient with absent dorsalis pedis and posterior tibial artery pulses after a road traffic absent also has no sensation below his knee, and his leg was internally rotated. What is the likely cause?
- Neck of femur fracture
- Posterior hip dislocation with sciatic nerve injury::✔
- Anterior hip dislocation
- Fracture distal femur
- A patient in a car crash struck the back of the driver’s seat, with a shortened, internally rotated leg, complete motor loss, and only preserved sensation on medial leg and foot. Diagnosis?
- Posterior hip dislocation::✔Classic for posterior dislocation: Limb is shortened, adducted, internally rotated
- A man suffered a fracture of the neck of the femur. An ORIF was done through a posterior hip approach. Postoperatively, he complained of weakness in his left leg. Diagnosis?
- Sciatic nerve injury::✔
Sciatic nerve runs close to the posterior hip and is at risk during surgery and posterior thigh trauma. Sciatic nerve injury causes motor loss in hamstrings, and weakness of dorsiflexion, and eversion with foot drop due to the peroneal division. Sciatic nerve injury also causes sensory loss over the posterolateral leg and dorsum of foot.
- A man in an accident has an entry wound on the posterolateral aspect of the left thigh and an X-ray reveals a bullet adjacent to the femur. He is not able to move his left toes or ankle. Which is the likely nerve lesion?
- S1 root lesion::Less likely with localised thigh trauma
- L5 root lesion::Would not affect all foot/toe movement
- Deep peroneal nerve palsy::Only dorsiflexion affected, causes foot drop, not plantar issues
- Sciatic nerve palsy::✔Sciatic runs posterior thigh, likely involved in penetrating trauma
- Tibial nerve palsy::Plantarflexion only affected
- Which of the following statements is accurate about the sciatic nerve?
- It is a single trunk above the piriformis
- It is a single trunk above & 2 trunks below the piriformis
- It is a single trunk below & 2 trunks above the piriformis
- It is a single trunk below the piriformis::✔
The sciatic nerve exits the pelvis through the greater sciatic foramen and passes as a single trunk below the piriformis.
- A patient sustains a lower limb trauma after an RTA. On examination, both dorsalis pedis and posterior tibial pulses are absent. Which fracture is most likely responsible?
- Supracondylar femur::Popliteal artery injury, but distal pulses may still be felt depending on collateral flow
- Midshaft of tibia::✔
- Lateral malleolus::May cause local arterial spasm but unlikely to abolish both distal pulses
- Neck of femur::May compromise femoral head blood supply leading to AVN
- Femoral epicondyle::Unlikely to cause loss of both distal pulses
Tibial shaft fractures can injure the anterior tibial or posterior tibial arteries, leading to absent dorsalis pedis and posterior tibial pulses.
- The superior gluteal nerve passes above which muscle and through which foramen?
- Piriformis::✔
The superior gluteal nerve exits the pelvis via the greater sciatic foramen and passes above the piriformis muscle to enter the gluteal region, where it travels between the gluteus medius and minimus supplying both. Its function is hip abduction and medial rotation, with injury causing Trendelenburg gait due to weak hip abduction.
- A patient is unable to medially rotate the thigh. What is the affected nerve?
- Superior gluteal nerve::✔Innervates gluteus medius and minimus, medial rotators and abductors of the thigh
- Inferior gluteal nerve
- Sciatic nerve
- Pudendal nerve
- A 73-year-old man presents with pain in the right buttock. Clinical examination reveals weakness of abduction of the right thigh. What is the most likely nerve to have been affected?
- Inferior gluteal
- Nerve to obturator internus
- Nerve to quadratus femoris
- Superior gluteal nerve::✔Innervates gluteus medius and minimus, medial rotators and abductors of the thigh
About the superior gluteal nerve:
- Arises from the L4,L5,S1 nerve roots (sacral plexus)
- Exits the pelvis via the greater sciatic foramen
- Passes above the piriformis muscle
- Runs between the gluteus medius and gluteus minimus
- Innervates:
- Gluteus medius
- Gluteus minimus
- Tensor fasciae latae
- Function: Hip abduction and medial rotation; injury causes Trendelenburg gait due to weak hip abduction.
- A 54-year-old man underwent hip replacement for a fractured neck femur. During follow-up, the man walks with the Trendelenburg gait. What is the most likely cause?
- Femoral nerve injury::Weak hip flexion, knee extension, not Trendelenburg
- Sciatic nerve injury::Foot drop, posterior leg sensory loss
- Inferior gluteal nerve injury::Weak gluteus maximus (hip extension), not abduction
- Injury to the superior gluteal nerve::✔
- A 53-year-old man presented with difficulty in hip abduction with an evident waddling gait during walking. An injury to which structure would produce this clinical picture?
- Superior gluteal nerve::✔
- A 73-year-old man presents with pain in the right buttock. Clinical examination reveals weakness of abduction of the right thigh. What is the structure most likely to have been affected?
- Superior gluteal nerve::✔
- Which artery originates from the internal iliac artery and exits through the greater sciatic foramen above the piriformis muscle and then bifurcates into the superficial and deep branches?
- Superior gluteal artery::✔Superior gluteal artery, vein and nerve exit via the suprapiriform greater sciatic foramen
- During a posterior hip approach for a fractured neck of femur, bleeding occurred and the surgeon tried to control the bleeder with ligation. Which blood vessel is mostly injured?
- Femoral artery::Located anteriorly
- Superior gluteal artery::Exits above the piriformis so unlikely to be injured unless very superior dissection
- Saphenous vein::Located medially and distally, unrelated to hip surgery
- Inferior gluteal artery::✔
The inferior gluteal artery arises from the anterior trunk of the internal iliac artery, and exits the pelvis through the greater sciatic foramen below the piriformis and thus is at risk during posterior hip surgeries.
The superior gluteal artery arises from the posterior trunk of the internal iliac artery, and exits the pelvis through the greater sciatic foramen above the piriformis.
The greater sciatic foramen is divided by the piriformis muscle into the suprapiriform and infrapiriform foramina.
- Suprapiriform greater sciatic foramen:
- Superior gluteal nerve, artery and vein
- Infrapiriform greater sciatic foramen:
- Posterior femoral cutaneous nerve
- Sciatic nerve
- Pudendal nerve
- Inferior gluteal nerve, artery and vein
- Nerve to obturator internus
- Nerve to quadratus femoris
Lesser sciatic foramen:
- Leave the pelvis via the greater sciatic foramen, then re-enters via the lesser sciatic foramen
- Pudendal nerve
- Internal pudendal artery
- Internal pudendal vein
- Nerve to obturator internus
- Obturator internus tendon
- A patient undergoes leg surgery under spinal anaesthesia. The block reaches up to the umbilicus. Which dermatome corresponds to this level?
- T8
- T10::✔Umbilicus is the classic landmark for the T10 dermatome
- T12
- L1
- A footballer develops sudden posterolateral thigh pain while sprinting during football. On examination, he has tenderness in the lower lateral posterior thigh and cannot fully extend the knee due to pain. Diagnosis?
- Biceps femoris tear::✔
- Gastrocnemius tear::Calf muscle
- Gracilis tear::Medial thigh muscle, adductor
- Semimembranosus tear::Medial hamstring
- Semitendinosus tear::Medial hamstring
The biceps femoris is the most lateral hamstring muscle and is the most commonly injured hamstring muscle, especially prone to tearing in sprinting injuries and eccentric loading e.g. during deceleration. Injury causes very sudden posterolateral thigh pain, and pain on knee extension or weight bearing.
- Which muscle is primarily responsible for extension at the hip joint?
- Rectus femoris::Extends the knee, flexes the hip
- Iliopsoas::Primary hip flexor
- Semitendinosus::✔Hamstring muscle; hip extensor, knee flexor
- Sartorius::Hip abductor and flexior, knee flexor
- Which of the following muscles is a hip adductor?
- Semitendinosus::Medial hamstring muscle; extends hip, flexes knee
- Biceps femoris::Lateral hamstring muscle; knee flexor
- Gracilis::✔Gracilis, a superficial medial thigh muscle, adducts the hip and assists knee flexion
- Sartorius::Flexes, abducts, and externally rotates hip
- A middle-aged man presents with impotence and symptoms of vascular insufficiency in the lower limbs. Which vascular lesion is most likely responsible?
- Abdominal aortic aneurysm::Pulsatile abdominal mass
- Femoral artery stenosis::Unilateral claudication
- Bilateral common iliac artery occlusion::✔usually at the aortic bifurcation
- Renal artery stenosis::Hypertension, renal dysfunction
Leriche syndrome’s △: impotence, buttock/thigh claudication, absent/diminished femoral pulses
- A patient presents with unilateral buttock claudication. What is the most likely affected artery?
- Common iliac artery::✔Supplies both internal and external iliac; buttock claudication is from internal iliac ischemia
- A patient complains of calf claudication on walking short distances. On examination, tibial artery pulses are absent. What is the most likely site of arterial occlusion?
- Superficial femoral artery::✔Most common site of occlusion in PAD, causing calf claudication
Claudication
- Bilateral buttock and impotence → Leriche’s syndrome, at the aortic bifurcation and common iliac arteries
- Unilateral buttock/thigh → Common iliac artery
- Thigh → External iliac artery
- Calf → Superficial femoral artery
- A 65-year-old man presents to the emergency department with left thigh pain after walking a fixed distance. His pulses are intact on the opposite limb. What is the most likely site of stenosis?
- Common iliac artery::Typically causes buttock and hip claudication
- Internal iliac artery::Supplies the pelvis, not the thigh
- Femoral artery::Proximal; not the usual culprit for exertional thigh pain
- Profunda femoris artery::✔
The deep femoral artery / profunda femoris artery, is the main artery supplying blood to the thigh. It branches off the femoral artery and gives rise to the medial and lateral circumflex femoral arteries, which supply the medial and lateral thigh and hip muscles.
- During hip surgery, the surgeon releases the iliopsoas muscle near its insertion at the lesser trochanter. Which structure is most at risk of injury in this area?
- Femoral nerve
- Femoral artery
- Femoral vein
- Medial circumflex femoral artery::✔
- Sciatic nerve
The medial circumflex femoral artery runs posteriorly, coursing near the lesser trochanter, vulnerable during iliopsoas release or femoral neck fractures.
- A patient with a history of claudication now presents with night-time pain in the same limb, and a claudication distance of 1 km. The foot is warm, with brisk capillary refill, but non-palpable dorsalis pedis pulse. Diagnosis?
- Critical limb ischaemia::✔
- During a posteromedial approach to excise a Baker’s cyst, which structure in the neurovascular bundle is most superficial and susceptible to injury?
- Sciatic nerve::Higher in the thigh, splits above the popliteal fossa
- Saphenous vein::Most superficial, and is medial so at risk - but not ‘in the neurovascular bundle’
- Tibial nerve::✔Tibial n. is the most superficial of the popliteal neurovascular bundle
- Sural nerve::Lateral, superficial
- Common peroneal nerve::Runs laterally around the neck of the fibula
In the popliteal fossa, the neurovascular bundle structures from superficial to deep are:
- Tibial nerve → Popliteal vein → Popliteal artery.
- A 21‑year‑old man is stabbed in the popliteal fossa, dividing the popliteal artery, and repair is via a posterior approach. When dissecting deep from the skin, which structure is encountered first?
- Popliteal artery
- Popliteus muscle
- Popliteal vein
- Tibial nerve::✔Most superficial
- Soleus muscle
- A 65-year-old man with longstanding atrial fibrillation develops an embolus to the lower leg. The decision is made to perform an embolectomy, utilising a transpopliteal approach. After incising the deep fascia, which of the following structures will the surgeons encounter first on exploring the central region of the popliteal fossa?
- Popliteal vein
- Common peroneal nerve
- Popliteal artery
- Tibial nerve::✔
- A patient has an injury in the lower thigh causing the absence of plantarflexion. Which nerve is damaged?
- Tibial::✔The tibial nerve supplies the plantar flexors of the foot.
- A patient is unable to plantarflex his left ankle after a knife injury near the lower hip. Which nerve is injured?Common peroneal::Gives off the deep peroneal branch, which enables dorsiflexion
- Deep peroneal::Deep peroneal enables foot dorsiflexion
- Sural::Sural nerve is purely sensory to lateral foot/ankle
- Superficial peroneal::Superficial peroneal enables foot eversion
- Tibial nerve::✔Innervates calf muscles gastrocnemius and soleus for plantarflexion
- A patient was stabbed in the buttock during a fight. On examination, he has a deep wound with loss of plantarflexion of his foot and toes, but normal dorsiflexion. What is the most likely injured structure?
- Common peroneal::Would cause foot drop, from dorsiflexion loss
- Pudendal::Supplies perineum, not motor to foot
- Saphenous::Purely sensory
- Tibial component of sciatic nerve::✔Supplies posterior compartment (plantarflexion)
- Sural::Sural nerve is sensory only, from the medial aspect of leg
Loss of plantarflexion with preserved dorsiflexion suggests injury to the tibial component of the sciatic nerve, which innervates gastrocnemius and soleus muscles.
- A patient has sensory loss in the plantar aspect of his left medial 3 and a half toe. Which nerve is affected?
- Medial plantar::✔
- Terminal branches of the tibial nerve:
- (i) the medial calcaneal nerve innervating the heel
- (ii) the medial plantar nerve innervating the plantar aspect of the middle 3.5 toes, and
- (iii) the lateral plantar nerve innervating the plantar aspect of the lateral 1.5 toes.
- In the leg, which of the following structures is in closest proximity to the middle of the fibula and at risk of injury during a fibulectomy?
- Fibular (peroneal) artery::✔Peroneal a. courses near the posterior aspect of the fibula, vulnerable in fibulectomy
- Which structure lies deepest in the posterior compartment of the leg?
- Tibial artery
- Fibular (peroneal) artery::✔
- Tibial nerve
- Saphenous nerve
Fibular a. is a deep branch of the posterior tibial a. that runs deep along the medial fibula, covered by the flexor hallucis longus.
- What is the most lateral structure in the popliteal fossa?
- Common peroneal nerve::✔Common peroneal nerve is most lateral, running along the biceps femoris
- A 35-year-old man has foot drop after tibia fracture treated with cast. Which nerve is injured?
- Common peroneal::✔Wraps over the fibular neck so it is vulnerable to injury, resulting in foot drop
- A young man sustains a gunshot to the lateral side of the knee. Which structure is most likely to be damaged?
- Common peroneal nerve::✔
- A patient underwent perianal surgery in the Lloyd-Davies position (modified lithotomy). After the procedure, they complain of foot drop. Which nerve is injured?
- Common peroneal::✔As it winds around the fibular neck
Foot drop (loss of dorsiflexion) is caused by weakness of muscles supplied by the deep peroneal nerve. However, the more common injury site in surgery/positioning is compression of the common peroneal nerve as it winds around the fibular neck where it is vulnerable in lithotomy/Lloyd-Davies position due to stirrups. In the Lloyd-Davies position, prolonged pressure or stretch on the lateral aspect of the knee can injure the common peroneal nerve, leading to foot drop due to loss of dorsiflexion and eversion.
- During recovery from varicose vein surgery, a 35-year-old woman complains of weakness of dorsiflexion of the ankle. Examination reveals absent sensation over the dorsum of the foot. Which nerve is injured?
- Common peroneal::✔
- A patient develops anterior compartment syndrome of the leg. Which movement is most likely impaired?
- Hallux flexion::FHL, tibial n., deep posterior compartment
- Hallux extension::✔EHL, deep peroneal n., anterior compartment
- Ankle plantarflexion::Gastrocnemius/soleus, tibial n., superficial posterior compartment
- Foot eversion::Peroneus longus/brevis, superficial peroneal n., lateral compartment
- Foot inversion::Tibialis posterior, tibial n., deep posterior compartment
- A patient develops anterior compartment syndrome following a tibial fracture. Where is the site of sensory loss?
- First dorsal web space::✔First webspace is supplied by the deep peroneal n. in the anterior compartment
- A patient with fracture tibia in cast for 5 weeks develops severe pain in the leg with pain on plantar flexion. Where would you expect sensory loss?
- First web space::✔The deep peroneal n. is stretched by plantar flexion of toes
- A man described loss of sensation in the first web space of the left foot. Which nerve is injured?
- Deep peroneal::✔The deep peroneal (fibular) nerve innervates the first interdigital cleft
- During recovery from varicose vein surgery, a woman complains of weakness of dorsiflexion and eversion of the ankle. Examination shows absent sensation over the dorsum of the foot. Which nerve is most likely injured?
- Deep peroneal nerve::Foot drop (dorsiflexion weakness) but sensory loss only in 1st dorsal webspace?
- Saphenous nerve::Sensory only
- Common peroneal nerve::✔Supplies eversion and dorsiflexion, and sensation from dorsum of foot
- Sural nerve::Sensory only
- A farmer sustains a deep 2 cm long laceration to the lateral aspect of the lower leg, anterior to the lateral malleolus. Which of the following structures is most at risk of being divided?
- Peroneus brevis::Posterior to lateral malleolus
- Peroneus longus::Posterior to lateral malleolus
- Saphenous nerve::Anterior to the medial malleolus
- Superficial peroneal nerve::✔Anterior to the lateral malleolus
- Sural nerve::Posterior to lateral malleolus
- A patient loses foot eversion after a fibular fracture. Which nerve is injured?
- Superficial peroneal::✔Superficial peroneal n. innervates the evertors: peroneus longus and peroneus brevis
- Common peroneal → Dorsiflexion + Eversion; Sensory: Dorsum of foot
- Superficial peroneal → Eversion via peroneus longus & brevis; Sensory: Dorsum of foot except 1st webspace
- Deep peroneal → Dorsiflexion via tibialis anterior, EHL, EDL; Sensory: Dorsal 1st webspace
- In a postero-lateral surgical approach to the ankle, which nerve is most at risk of injury?
- Sural nerve::✔
- A man has loss of sensation over the lateral aspect of his leg after varicose vein surgery. Which nerve is injured?
- Sural::✔Lateral lower leg sensation and no motor disruption: Sural nerve
- A surgical incision is made at the lateral side of the foot. Which nerve is most at risk of injury?
- Sural::✔
The sural nerve runs behind the lateral malleolus, together with the small saphenous vein. It is sensory only, supplying the posterolateral leg, lateral heel, ankle, and foot. During a posterolateral approach to the ankle (commonly used for fixation of posterior malleolar fractures), the sural nerve is the structure most likely to be injured.
- A 30‑year‑old man suffers a knee dislocation reduced under anaesthesia, then has a sciatic block and is noted to have a painless, pulseless limb. Which structure is injured?
- Popliteal artery::✔Posterior knee dislocations injure the popliteal artery, hence pulseless; pain-free per the block
- Which structure is most at risk when preparing tibia with saw during knee replacement?
- Common peroneal nerve::✔
- Which structure is most at risk during posterior capsule release, retractor placement, or cement pressurisation?
- Popliteal artery::✔
- A patient with popliteal artery stenosis develops acute limb ischemia. What is the most likely underlying cause?
- Thrombosis::✔Chronic stenosis predisposes to in-situ thrombosis, which can suddenly occlude the artery.
- Emboli
- Atheroma
- Vasculitis
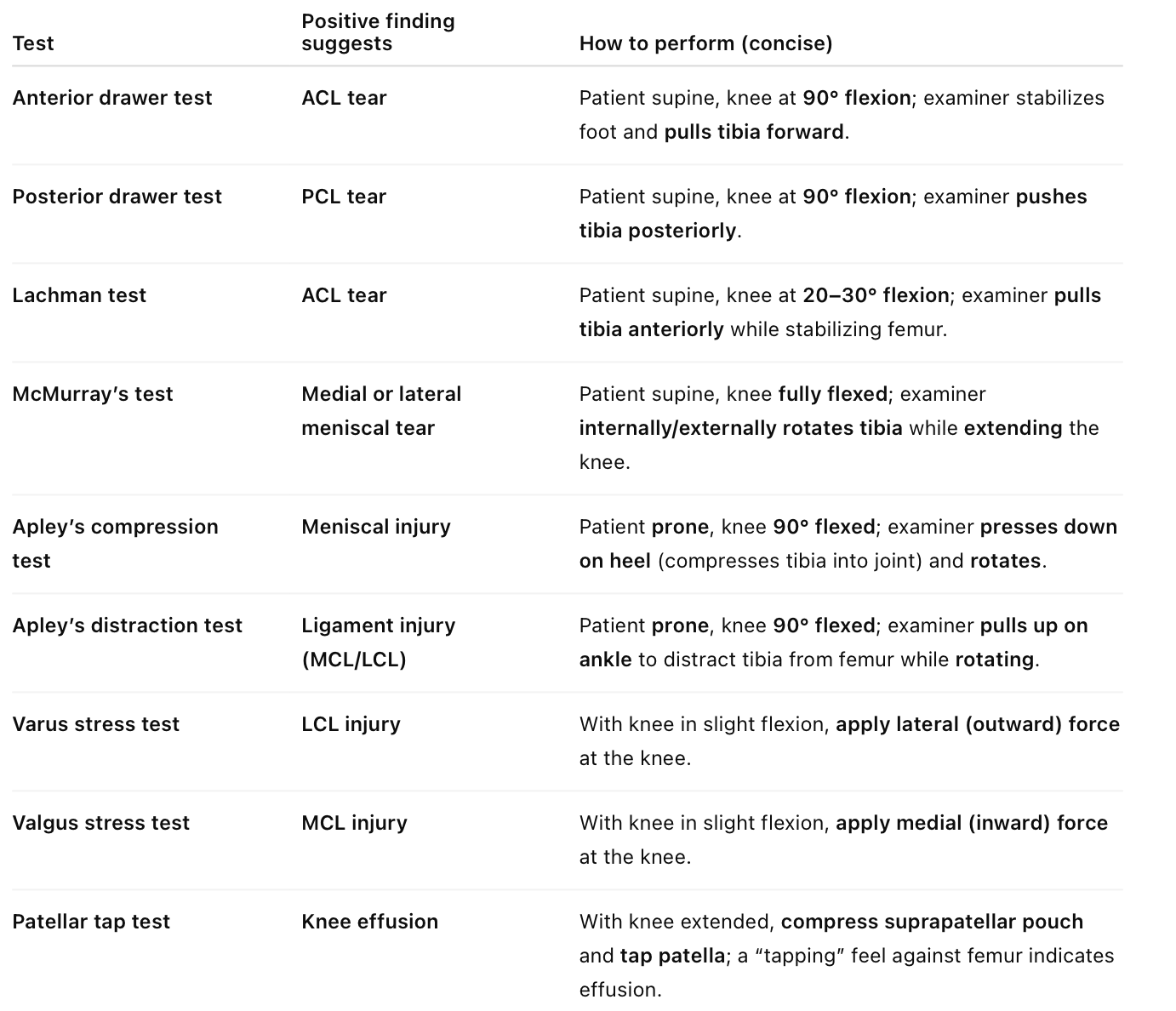
Testing for knee injuries
- A footballer presents after a knee injury. Anterior drawer test is positive, McMurray test is negative. Diagnosis?
- ACL injury::✔
- Meniscal tear::Positive McMurray
- PCL injury::Positive posterior draw test
- Loose body::Would cause intermittent locking with sharp pain
- MCL injury::Positive valgus stress test
- A patient who suffered a knee injury is positive for the anterior drawer test. Which ligament is injured?
- ACL::✔
- A young footballer injures his knee during a match. Hours later, he develops swelling and inability to extend the knee. MRI likely shows:
- ACL injury::✔ACL injuries cause hemarthrosis, swelling in hours and can restrict motion
- A 25-year-old man sustains a twisting injury while playing football. He develops immediate knee swelling and is unable to continue playing. Six months later, his knee still feels unstable and gives way. On examination, he has full range of motion, a small effusion, and a positive anterior drawer test. What is the most likely structure damaged?
- ACL::✔Positive anterior drawer test, immediate swelling, instability, inability to continue pivoting activities
- A young woman crashes into soft snow while skiing. She experiences sudden knee swelling, a positive patellar tap, and difficulty extending her knee. Aspiration confirms hemarthrosis. Diagnosis? ACL rupture::✔Non-contact twisting injuries like skiing falls; △ of pop, rapid joint swelling and instability
- A female skier presents with sudden severe knee pain and swelling. A large hemarthrosis is drained. Diagnosis?
- Complete tear of ACL::✔Common cause of acute hemarthrosis
- A 25‑year‑old footballer cannot actively extend his left knee after a twisting injury. Which structure is likely torn?
- ACL::✔Tear leads to instability and inability to extend under load
- A 30-year-old man injures his knee in a road traffic accident. Later, the tibia is posteriorly displaced in comparison to the opposite leg. What structure is likely injured?
- PCL::✔Posterior sag sign and difficulty walking downhill suggest PCL rupture
- A tennis player injured his knee. On examination, his left tibia is positioned posterior to the femur. Diagnosis?
- PCL injury::✔
- A young girl presents with anterior knee pain, especially when walking up or down stairs. Diagnosis?
- Osgood-Schlatter disease::More common in active adolescents with tibial tuberosity pain
- Patellar tendonitis::Typically causes pain just below the kneecap, worsens with jumping
- Chondromalacia patella::✔Softening of the cartilage under the patella; worse climbing stairs
- Meniscal tear::Usually involves joint line pain, swelling, and clicking
- ACL tear::Presents with instability, not isolated stair pain
- Chondromalacia patella / patellofemoral pain syndrome, is common in young females and causes anterior knee pain worsened by stairs, squatting, or sitting for long periods.
- A footballer sustained a knee injury in a match and has a positive valgus stress test and minimal joint effusion. Which structure is most likely injured?
- Medial collateral ligament::✔Positive valgus test, localized pain and swelling
- A footballer injures his knee and cannot continue playing. One week later, he has tender swelling 2.5 cm above the medial joint line and excessive lateral angulation of the knee. Which structure is most likely injured?
- Medial collateral ligament::✔Valgus stress injury, tenderness over medial joint line, valgus deformity
- A 19‑year‑old athlete injured his left knee during a fight. On examination, there’s maximal tenderness when pushing the knee from lateral to medial. Which structure is most likely injured?
- Lateral collateral ligament::✔Varus stress (lateral‑to‑medial force) reproduces LCL pain
- A 30‑year‑old man’s knee is locked in 30° of flexion after a twisting injury; he cannot actively flex or extend further, though the knee “gives way” when he leans on it. Diagnosis?
- Bucket handle meniscal tear::✔
Bucket‑handle meniscal tears create a mechanical block, “locked knee” and episodes of giving way. The torn meniscus flips into the joint, “locking” the knee at a fixed angle; it may transiently yield, “give way”, when pressure is applied.
- During a football game, a player sustains a twisting knee injury. The next day, examination reveals a positive patellar tap and inability to extend the knee. Diagnosis?
- Bucket handle meniscal tear::✔Athlete with twisting flexed knee injury, mechanical block to extend
- During football, a player twists his knee. The next day he has a patellar tap. Four weeks later, after another twist he again develops swelling. Diagnosis?
- Medial meniscal tear::✔Causes delayed joint effusion after twisting injury and recurs with further minor trauma
- Twisting injury during football → Could injure ACL or meniscus
- Immediate swelling (< 6h) → Ligament rupture (ACL, PCL) or patellar dislocation
- Delayed/recurrent swelling (24-48h, after activity) → Meniscal tear
- A 25-year-old footballer injured his left knee. Four weeks later, he returned to play and reinjured it. On examination, he cannot extend the knee. What is the most likely cause?
- Loose body secondary to osteochondritis dissecans::✔
- A 65‑year‑old man with progressive osteoarthritis can’t extend his knee. There is no history of trauma. Diagnosis?
- Loose body::✔
- Degenerative loose bodies, formed from osteoarthritic cartilage or osteophyte fragments, can arise in osteoarthritic joints and mechanically block knee extension even without an acute injury.
- A woman has a slowly growing, painful lateral swelling at the knee, with no trauma history. Diagnosis?
- Meniscal cyst::✔
Meniscal cysts form from synovial fluid extrusion through a torn meniscus; they present in the lateral knee as painful, fluid filled swellings that fluctuate in size.
- A 25-year-old woman presents with spontaneous haemarthrosis of her left knee. Lab tests show normal PT and elevated APTT. What is the most likely cause?
- Factor VIII deficiency::✔This is haemophilia A, with elevated APTT and normal PT
- A patient has calf pain on hip movement and a weak distal pulse below the knee. What is the most likely cause?
- Embolus::✔Sudden limb ischaemia with pain and weak distal pulses indicates arterial embolismAcute arterial embolus presents with sudden pain, pulselessness and limb ischaemia requiring prompt embolectomy.
- A young woman suddenly felt a sharp pain in the back of her ankle while walking and collapsed. Which clinical test is expected to be positive?
- Phalen test::Used in carpal tunnel syndrome
- Simmonds-Thompson test::✔Achilles tendon rupture: Calf squeeze fails to produce plantar flexion
- Froment test::Assesses ulnar nerve palsy and adductor pollicis weakness
- Retropulsion test::Used for postural instability in Parkinson’s disease
- A 45-year-old woman playing tennis feels sudden pain in the back of her ankle, like being hit. What is the most appropriate test?
- An impingement sign::Ankle impingement (bony or soft tissue)
- Phalen's manoeuvre::Carpal tunnel syndrome; wrist flexion induces symptoms
- Simmonds’ squeeze test::✔The feeling "like being kicked" in the back of the leg is characteristic
- Thomas test::Hip flexion deformity, typically due to tight iliopsoas or hip joint pathology.
- A patient presents with sudden heel pain and is unable to bear weight, and a positive Simmonds test. Diagnosis?
- Achilles tendon rupture::✔Loss of plantar flexion with positive Simmonds (Thompson) tesT
Simmonds’ (Thompson) test is used to assess Achilles tendon rupture. The patient lies prone with feet hanging off the edge of the bed. When the calf is squeezed, absence of plantarflexion indicates tendon rupture.
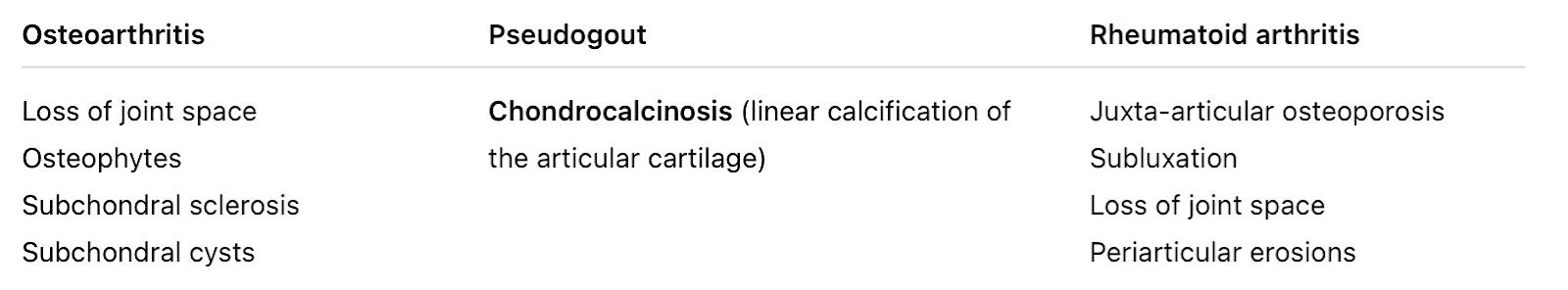
- A man presents with first metatarsal pain. X-ray shows reduced joint space and subchondral cysts. Diagnosis?
- Osteoarthritis::✔Joint space narrowing with subchondral cysts are classic OA findings.
- A 10-year-old boy with a history of midtarsal dislocation now presents with worsening foot pain. Diagnosis?
- Malunion::Less likely this late unless poorly treated initially
- Avascular necrosis::AVN is less common in midfoot long-term
- Primary osteoarthritis::Not typical in a child
- Secondary osteoarthritis::✔Joint damage from trauma leads to post-traumatic arthritis
Secondary (post-traumatic) osteoarthritis is a common long-term complication of midtarsal injuries, especially if the joint surfaces were not well aligned or if cartilage damage occurred.
- A man had pinning for a metatarsal fracture 20 years ago. He now suffers pain and stiffness at the site. Diagnosis?
- Malunion::May cause deformity and pain, but stiffness decades later points to joint degeneration
- Nonunion::Would present with persistent pain earlier, not stiffness
- Avascular necrosis::In metatarsal heads, rare and earlier presentation
- Osteoarthritis::✔Post‑traumatic joint degeneration develops over years
- Sudeck’s atrophy::Complex regional pain syndrome
Post‑traumatic osteoarthritis often appears years after an injury or fixation, causing joint pain and stiffness.
- A 30‑year‑old athlete has sharp dorsal foot pain radiating into the toes, with a tender swelling between the 3rd and 4th metatarsals. What is the most likely cause?
- March fracture::Stress fracture of metatarsal shafts, not interdigital swelling
- Freiberg disease::Avascular necrosis of metatarsal head, not interdigital swelling
- Osteoarthritis::Would affect joint spaces, not a focal interdigital mass
- Morton’s neuroma::✔
- What is the expected histological finding of Morton's neuroma?
- Ischemic neuritis
- Necrosis of perineuritic tissue
- Fibrotic granuloma affecting perineuritic tissue::✔
- Benign tumor affecting the nerve
- Which of the following pathological features is characteristic of Morton’s neuroma?
- Multiple ectatic vascular structures::Seen in vascular malformations
- Nerve bundles associated with fibrosis::✔Classic finding in Morton neuroma
- Cells suggestive of a fibromatosis::Dupuytren’s or plantar fibromatosis
- Wallerian degeneration::Nerve transection or severe axonopathy
Morton’s neuroma is a perineural fibrosis of the plantar digital nerve, most often occurring between the 3rd and 4th toes. It typically presents as forefoot pain and tenderness between the metatarsal heads, sometimes felt as a lump, and is often relieved by removing shoe pressure.
- A 30-year-old patient sustained a subcapital fracture of the femur, managed with closed reduction and had an excellent initial prognosis. One year later, he presents with hip pain and stiffness. Diagnosis?
- Avascular necrosis::✔
- Malunion::Intertrochanteric/extracapsular fractures leading to deformity and abnormal biomechanics
- Nonunion::Manifests within months with persistent pain and lack of healing
- Osteoarthritis::Can occur secondarily, but one year is too early without preceding AVN or cartilage loss
- A patient develops hip pain months to years after pinning for a femoral neck fracture. What is the likely cause?
- Avascular necrosis::✔Late complication due to damage of retinacular vessels
- Non-union::Presents earlier with persistent pain and failure of healing, not years later after initial union
- Malunion::Intertrochanteric/extracapsular fractures leading to deformity and abnormal biomechanics
Main arterial supply of the femoral head are retinacular branches of the medial circumflex femoral artery, along the femoral neck beneath the capsule. Intracapsular especially subcapital fractures may disrupt these vessels. In adults, the artery of ligamentum teres from the obturator artery provides minor supply though it provides enough in kids. If retinacular supply is cut and ligamentum teres are insufficient, avascular necrosis of the femoral head develops.
- A patient presents with a fibrotic mass on the plantar surface of the foot that is painful. On excision, tissue revealed a central bony calcification. What is the most likely pathological process?
- Atrophy
- Dysplasia
- Metaplasia::✔Fibroblasts in fibrous tissue undergo osseous metaplasia leading to bone formation in abnormal site
- Hypertrophy
- A 35-year-old patient has a previous scar on his big toe. A swelling develops under the scar. Histopathology of the swelling shows dense fibrous tissue with bone elements and calcification. What is the underlying process?
- Neoplasia
- Metaplasia::✔
- Hyperplasia
- Dysplasia
- Anaplasia
Osseous metaplasia is the transformation of noneosseous soft tissue into bone, as mesenchymal cells (like fibroblasts) differentiate into osteoblasts, typically due to chronic inflammation or repeated trauma. It's an adaptive non-neoplastic process.
- A 53‑year‑old female presents with a painful left knee. X‑ray reveals a huge lytic lesion in the tibia extending to the subchondral plate. Diagnosis?
- Osteosarcoma::Osteosarcoma → Metaphysis of long bones, mixed sclerotic and lytic, sunburst
- Ewing sarcoma::Ewing sarcoma → Diaphyseal “onion‑skin” periosteal reaction, children
- Giant cell tumour::✔Giant cell tumour → Epiphyseal, lytic “soap‑bubble” lesion extending to subchondral bone
- Osteomalacia::Osteomalacia → Causes pseudofractures, not focal lytic lesions
Giant cell tumours occur at the ends (epiphysis) of long bones, producing lytic lesions that abut the subchondral plate.
- What is the correct technique for tourniquet use during surgery?
- Inflation of cuff above diastolic after exsanguination
- Inflation of cuff above mean pressure before exsanguination
- Inflation of cuff above systolic before exsanguination
- Inflation of cuff above systolic after exsanguination::✔
Exsanguinate the limb (e.g. Esmarch bandage), then inflate cuff to > systolic pressure to reliably occlude arterial flow.
Correct Technique for Surgical Tourniquet:
- Exsanguinate the limb, usually with Esmarch bandage or elevation
- Then inflate the tourniquet cuff to:
- ≥ 100 mmHg above systolic for lower limb
- ~ 50 mmHg above systolic for upper limb
- This ensures a bloodless surgical field and minimizes pain and complications.
- A 34-year-old patient undergoes surgery with a tourniquet applied. After release of the tourniquet, vasodilation is observed. Which substance is most likely responsible for this effect?
- Noradrenaline::Causes vasoconstriction
- Vasopressin::A potent vasoconstrictor, released in response to hypotension
- Histamine::✔Released during reperfusion and leads to vasodilation and increased vascular permeability
- Serotonin::Causes vasoconstriction
Tourniquet release causes reperfusion injury, during which histamine is released from mast cells and damaged tissues. This leads to vasodilation, flushing, hypotension, and a transient drop in systemic vascular resistance. Other mediators include prostaglandins and nitric oxide.
- A 23‑year‑old man has intramedullary nailing of a femoral shaft fracture. At the end of surgery his lower leg is pale with a diminished pulse. What is the best next step?
- Re‑explore the wound::✔Urgent surgical exploration for vascular injury
- Angiography::Delays definitive management
- Embolisation::Not indicated without imaging first
- Compartment release::Pulses absent suggest likely arterial injury, not compartment syndrome
- Compression ultrasound::Too slow for an acute vascular emergency
Absent pulses and pallor immediately post‑fixation indicate arterial compromise, requiring prompt exploration.
- A patient with a right open femur fracture after an RTA develops a cold, numb, and pulseless limb despite resuscitation and traction. The traction is removed but perfusion does not return. What is the best next step?
- Surgical exploration of superficial femoral artery::✔
- CT angiogram
- Calf fasciotomies
- A 23-year-old athlete had his tibia fractured and was managed with an above-knee cast. He later developed severe pain. After cast removal, the skin appeared shiny, tense, and pale. Diagnosis?
- Compartment syndrome::✔
- Complex regional pain syndrome::Chronic, more widespread
- Hypovolemic shock::Not localised to one limb
- Cellulitis::Involves warmth, redness, and fever
Compartment syndrome is a surgical emergency. Increased pressure within a muscle compartment impairs blood flow, leading to tense swelling, pale shiny skin, pain out of proportion, and potential neurovascular compromise.
- A 45 years old patient sustained a tibial shaft fracture for which he underwent internal fixation. Now he complains of severe pain and paresthesia in his leg. His distal pulses are palpable. What is the first option for management?
- Fasciotomy::✔Classic presentation of compartment syndrome
- Escharotomy::Used for circumferential burns
- Analgesia::Does not treat underlying issue
- Immediate re-exploration::Fasciotomy is specific intervention
- Reassurance::Can lead to ischemia
- A patient had tibia and fibula fractures, was operated on, and is now in the ward with severe pain. What is the next step in management?
- Release 4 compartments::✔Fasciotomy if compartment syndrome is strongly suspected
- Measure intracompartmental pressure
- Pulse oximeter on great toe
- A patient is diagnosed with lower leg compartment syndrome. What is the correct surgical management?
- 4 compartment release::✔Anterior, lateral, superficial posterior, and deep posterior compartments
Pain out of proportion with paresthesia and intact pulses is characteristic of compartment syndrome. The patient requires an urgent fasciotomy.
- Which is the least reliable sign of compartment syndrome?
- Increasing pain out of proportion::Early and reliable
- Altered sensation::Early neurogenic sign
- Increased compartment pressure::Direct measurement, reliable
- Pain on passive stretch::Very sensitive
- Loss of dorsalis pedis pulse::✔A late and inconsistent sign—pulses often remain palpable until very late
Pulse loss is a late finding in compartment syndrome; relying on it delays diagnosis and can risk permanent damage.
- A 35-year-old presents with a pulseless right leg on extension, but a bounding popliteal pulse on the other side. No history of vascular disease. Diagnosis?
- Popliteal artery entrapment syndrome::✔
Popliteal artery entrapment syndrome is seen in young athletic males, with positional ischemia due to anatomical compression from abnormal muscle insertion.
- A 22‑year‑old athlete has intramedullary nailing of a tibial fracture. Seven hours later he develops sudden dyspnea, chest pain, and confusion. Diagnosis?
- Fat embolism::✔Classic timing is 1 to 3 days post long‑bone injury/surgery
- A patient sustains a femoral shaft fracture. Soon after, he develops respiratory distress, neurological signs, and bilateral petechial hemorrhages in the brain. What is the most likely diagnosis?
- Pulmonary embolism::Dyspnoea, chest pain
- Air embolism::Seen after neurosurgery/central line
- Fat embolism::✔△ respiratory distress, neurology, petechial hemorrhages in lungs, brain, skin
- Septic embolism::Associated with endocarditis
- Intracranial hemorrhage::Would not cause lung involvement
- An elderly man who suffered bilateral femur shaft fractures underwent fixation. Intra-operative blood loss was 800ml, and 1 hour post operatively he became tachypneic and then arrested. Diagnosis?
- Fat embolism::✔
Fat embolism syndrome typically presents 12 to 72 hours after long bone trauma but can occur earlier, especially in bilateral femur fractures. It manifests with respiratory distress, neurological symptoms, and petechial rash (late sign). Sudden hypoxia and arrest post-op in this setting is highly suggestive. Imaging may be normal or show ground-glass changes. Management is supportive, with early fracture fixation and DVT prophylaxis.
- A male with bilateral femur fractures from an accident is intubated. On day 10, he suddenly deteriorated with petechial haemorrhages. Labs show normal Hb, low fibrin, low platelets, and PT > 60 seconds. Diagnosis?
- Disseminated intravascular coagulation::✔
- A patient is admitted after a road traffic accident and undergoes splenectomy. He later develops a petechial rash, with low platelets, low haemoglobin, low fibrinogen, and prolonged PT and APTT. Diagnosis?
- Disseminated intravascular coagulation::✔
- Idiopathic thrombocytopenic purpura::Causes isolated thrombocytopenia; coagulation profile is normal
- Sepsis::Can trigger DIC, alone does not explain coagulation abnormalities
- Aplastic anaemia::Causes pancytopenia, but not coagulation abnormalities
- Herpes zoster::Causes painful vesicular rash in a dermatomal distribution
DIC: A consumptive coagulopathy triggered by trauma, sepsis, massive transfusion, or malignancy. DIC is characterised by consumption of platelets and clotting factors, leading to thrombocytopenia (↓Plt), ↓ fibrinogen, ↑PT, ↑APTT, anaemia (↓Hb) due to microangiopathic haemolysis, and bleeding signs e.g. petechiae.
- Which ligament is most commonly injured in an ankle inversion injury?
- Anterior talofibular ligament::✔Ankle’s weakest lateral ligament, most prone to sprain in inversion
Mnemonic: Anterior TaloFibular ligament Always Tears First; Calcaneofibular ligament Can follow
- A 23‑year‑old sustains an inversion ankle injury. Which two ligaments are most commonly injured?
- Anterior talofibular & calcaneofibular::✔
- An inversion ankle injury is the most common ankle sprain mechanism. It stresses the lateral ligament complex, which includes:
- Anterior TaloFibular ligament; most commonly injured Always Tears First
- Calcaneofibular ligament; second most common. Can follow
- Posterior Talofibular ligament; least commonly involved, usually in more severe injuries or dislocations.
- The sinus tarsi is located between which two bones?
- Calcaneus and talus::✔
- Sinus tarsi is a small, funnel-shaped space on the lateral side of the foot, between the calcaneus and the talus, anterior to the lateral malleolus. It contains soft tissues like ligaments, nerves, blood vessels, and fat. Sinus tarsi syndrome describes inflammation or injury to the tissues causing pain and instability in the outer ankle and hindfoot.
- The distal articular surfaces of the cuboid bone include:Fourth & fifth metatarsals::✔Cuboid articulates distally with the fourth and fifth metatarsals Medial cuneiform & navicular::Cuboid is lateral, not medialFirst & second metatarsals::Too medialTalus bone::Articulates proximally with calcaneus and navicularThird metatarsal bone::Interfaces via lateral cuneiform, not directly
- A 23-year-old athlete injured his ankle during a rugby game. The ankle X-ray was normal, but the pain persists. What is the most appropriate next step?
- Ankle MRI::✔Best for soft tissue and ligament injuries
- Repeat X-ray
- Ankle CT scan
- Discharge and review
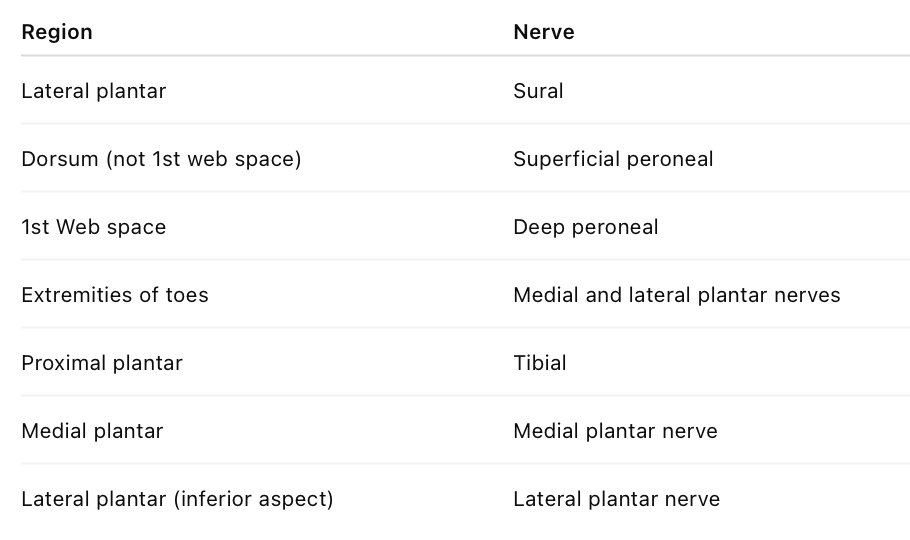
Cutaneous sensation of the foot