Burns Injury
wA 45-year-old male rescued from a fire in a closed room presents with multiple burn areas. Before entering, you must calculate the Total Body Surface Area (TBSA). Inside, you will be required to initiate immediate burn management based on your calculation. The patient weighs 70 kg and has sustained second-degree and third-degree burns to the anterior chest, entire right arm, anterior surface of the left leg and groin area.
How do you calculate the surface area of the burn?
The anterior chest is 36/2/2 (9), right arm is (9), anterior surface of the left leg is 18/2 (9) and groin area is (1) = 28%.
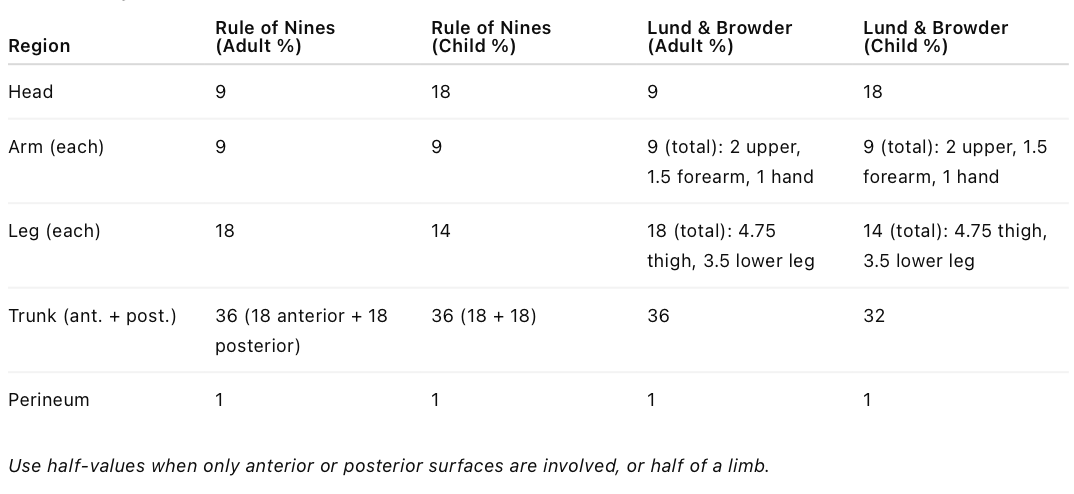
The two methods are according to the Wallace Rule of Nines or the Lund & Browder. For adults - The (anterior and posterior chest and abdomen) trunk is 36, each leg is 18, each arm is 9, the head is 9 and perineum is 1.
How would you manage this patient?
ATLS approach:
A – Airway with C-spine control
- High-flow oxygen please comp plea
- In a closed-space fire there is high risk of inhalation injury; Look for signs of airway burns and inhalation injury (soot, hoarseness, singed nasal hairs, stridor, facial burns) as it may cause airway oedema
- Early intubation airway oedema due to closed-space fire suspected
B – Breathing
- RR, SpO₂
- ABG including carboxyhaemoglobin level
- Consider cyanide poisoning if severe smoke inhalation
- Ensure adequate ventilation can be achieved; tracheal or pulmonary burns can impair effective gastric exchange and circumferential chest burns may require escharotomy to allow ventilation
C – Circulation
- Two large-bore IV cannulas
- Begin crystalloid (Hartman's / Ringers' lactate) resuscitation using the Parkland formula: 4 mL × (weight) kg × 28% = mL in 24 h; Give half in the first 8 hours from the time of the injury, and the second half in the following 16 hours; avoid colloids and deduct fluids already given
- Insert Foley catheter
D – Disability
- GCS
- Glucose
- Pupils
E – Exposure
- Remove clothing and jewellery
- Avoid hypothermia using warm ambient temperature, clean blankets, convection heaters, cling film
Secondary management
- Analgesia: IV opioids, Inhaled 70% nitrous oxide for acute pain
- Wound care: Cover burns with cling film or clean dry dressings; do not dress blisters; elevate limbs
- Stress ulcer prophylaxis: Start PPI or H2 antagonist
- Tetanus prophylaxis
- Escharotomy for circumferential chest and limb burns
- Begin early enteral feeding (within 6–12 hrs)
- Referral to burns centre if: TBSA >15%, inhalation injury, full-thickness, hands, face or perineum involvement etc.
- Ongoing monitoring of fluids, vitals, urine output
Why are colloids not given to burn patients?
- In the first 24 hours after burns, capillary permeability is massively increased.
- Colloids (e.g., albumin) leak out of vessels into the interstitial space.
- Their oncotic effect pulls even more fluid out of the circulation.
- This causes paradoxical third-space fluid accumulation, worsening oedema.
- Can worsen airway oedema in inhalation injuries.
- Therefore: use crystalloids only in first 24 h; colloids may be used later when capillary integrity improves.
How do you assess the adequacy of fluid therapy?
Clinical indicators
- Urine output (best marker): Aim UOP of 0.5 to 1 mL/kg/hr in adults
- Peripheral warmth
- CRT
- HR and BP
- Mental status
- Respiratory status
- Core temperature e.g. rectal temperature
Biochemical indicators
- Lactate and base deficit; improvement suggests adequate perfusion
- Haematocrit; but unreliable after transfusion or haemolysis
Invasive monitoring if available
- Central venous pressure and its response to fluid challenges
- Cardiac index / dynamic measures if in ICU
Avoid over-resuscitation:
- Look for pulmonary oedema
- Look for abdominal compartment syndrome
- Look for limb compartment syndrome
What are the potential complications of suffering burns injuries?
Early
- Burn shock: Hypovolaemia leads to ↓BP, ↑HR, ↑SVR, ↓CO
- Respiratory complications: Airway obstruction, CO poisoning, cyanide toxicity, ARDS
- Electrolyte abnormalities: ↓/↑Na, ↑K, ↓Ca
- Renal failure from hypovolaemia or pigment nephropathy
- Myoglobinuria / haemoglobinuria
- Coagulopathy due to DIC and hypothermia
- Sepsis
- Infection, cellulitis
- Compartment syndrome of the limbs or chest
Late
- Multi-organ failure
- Scarring and contractures
- Chronic pain
- Psychological trauma
- Hypermetabolic state
- Malnutrition
- Functional impairment
How can you tell if it is a superficial or a deep burn?
Superficial / partial-thickness
- Red or white
- Moist, blistering
- Painful / highly sensate
- Blanches on pressure
- Capillary refill present
- Heals without grafting
Deep partial-thickness or full-thickness
- White, black, or leathery
- Dry, waxy
- Insensate as nerve endings are destroyed
- No capillary refill
- Does not blanch
- Requires grafting