Neuro-Anatomical Localisation & Spinal Cord Syndromes
👩⚕️I think the best way to learn this is by working through MCQs so let's get right into it:
Which structure is primarily responsible for autonomic nervous system control?
- ((Thalamus::Relay station for sensory pathways to the cortex))
- ((Medulla::Contains vital reflex centres but is under hypothalamic control))
- ((Globus pallidus::Part of basal ganglia involved in motor regulation))
- ((Hypothalamus::💡 Regulator of autonomic, endocrine, and homeostatic functions))
Which function is lost in the event of injury to the dorsal root ganglion?
- ((Voluntary motor control::Mediated by corticospinal motor pathways))
- ((Autonomic regulation::Controlled mainly by hypothalamus and brainstem))
- ((Sensory perception::💡 Dorsal root ganglia contain cell bodies of first-order sensory neurones))
- ((Reflex motor output::Motor limb of reflex arc remains intact))
Cerebellar lesions
The cerebellum has two major zones: the midline vermis and lateral hemispheres - and injury to either zone results in different symptoms.
Vermis lesions lead to:
- Gait/truncal ataxia, with a broad‑based, unsteady gait
- Dysarthria, with slurred scanning explosive speech
- Nystagmus, gaze-evoked, or jerk nystagmus
Hemisphere lesions lead to:
- Dysdiadochokinesia, impaired rapid alternating movements of the limbs
- Intention tremor, decomposition of movement on goal‑directed tasks
- Limb ataxia
- Hypotonia
- Limb dysmetria, past-pointing
- Poor coordination on finger‑nose testing
A 55-year-old presents with an unsteady gait but no dysmetria or past-pointing. Which is the most likely site of the lesion?
- ((Posterior horn of spinal cord::Receives sensory afferents))
- ((Cerebellum::💡 Vermis lesions cause gait ataxia without limb dysmetria or past-pointing))
- ((Basal ganglia::Involved in initiation and modulation of movement))
- ((Upper motor neurone::Causes spastic weakness rather than ataxia))
Parkinsonism
Bradykinesia means slowness in starting and performing movements. Cogwheel rigidity feels like a ratchet-like catch when you passively move a patient’s limb. Along with a resting tremor, these are the classic signs of Parkinsonism.
The basal ganglia (striatum, globus pallidus, substantia nigra, and subthalamic nucleus) control movement through two systems:
- The direct pathway helps start and smoothen movements.
- The indirect pathway slows or stops movements.
Normally, dopamine from the substantia nigra boosts the direct pathway and inhibits the indirect pathway, allowing smooth motion. In Parkinson’s disease, dopamine-producing neurons die, so movement starts slowly (bradykinesia) and muscles become stiff (rigidity).
A 85‑year‑old develops cog‑wheel rigidity and bradykinesia. Which structure is most likely affected?
- ((Posterior horn of spinal cord::Receives sensory afferent fibres))
- ((Cerebellum::Coordinates movement and balance))
- ((Basal ganglia::💡 Involved in movement initiation and modulation; lesions cause rigidity and bradykinesia))
- ((Anterior horn of spinal cord::Contains lower motor neurone cell bodies))
Horner's syndrome
Horner’s occurs if the sympathetic supply to the eye and face is disturbed. These sympathetic fibres start in the hypothalamus, descend to synapse with preganglionic sympathetic neurons in the lateral horn of T1 to T4. From there, the fibres travel upward through the sympathetic chain, often passing through the stellate ganglion, a fused structure of the inferior cervical and first thoracic ganglia. Finally, they synapse in the superior cervical ganglion, where postganglionic fibres then continue to the eye, eyelid, and face. Damage to this pathway results in the △ ptosis, miosis and ipsilateral face anhidrosis - Horner's syndrome.
A 62-year-old post-hyperhidrosis surgery patient presents with ptosis, miosis, and anhidrosis (Horner’s syndrome). Which spinal cord region is affected?
- ((Anterior horn::Contains lower motor neurones only))
- ((Lateral horn::💡 Contains sympathetic preganglionic neurones running from T1 to L2))
- ((Posterior horn::Contains sensory relay neurones only))
- ((Dorsal root ganglia::Contains peripheral sensory cell bodies))
To treat hyperhidrosis the sympathetic ganglia at T2 and T3 are divided, risking causing Horner's.
A patient presents with ptosis, miosis, and anhidrosis, along with numbness over the medial side of the elbow. Which nerve root is most likely affected?
- ((C5::Involved in shoulder abduction))
- ((T1::💡 Involved in sympathetic supply to the eye (Horner’s) and medial arm sensation))
- ((C7::Supplies triceps and wrist extensors))
- ((T2::Rarely isolated))
A patient with a Pancoast tumour presents with wasting of the intrinsic muscles of the hand. Which nerve root is most likely affected?
- ((C5::Supplies deltoid and rotator cuff))
- ((C7::Supplies triceps and wrist flexors))
- ((T1::💡 Compression of brachial plexus roots (C8, T1) which supply intrinsic hand muscles))
- ((L5::Supplies ankle dorsiflexors))
A patient with a Pancoast tumour develops ptosis, miosis and anhidrosis. Where is the underlying injury?
- ((Vagus nerve::Parasympathetic innervation, not sympathetic))
- ((Recurrent laryngeal nerve::Causes hoarseness, not Horner’s))
- ((Sympathetic chain at T1::💡 Compression of stellate ganglion/sympathetic chain at T1))
- ((Phrenic nerve::Causes diaphragmatic paralysis, not Horner’s))
A patient undergoes treatment for hyperhidrosis. Horner’s syndrome is caused by injury to which ganglion in front of the neck near the 1st rib?
- ((Gasserian::Trigeminal sensory ganglion))
- ((Pterygopalatine::Parasympathetic relay from CN VII to lacrimal gland))
- ((Stellate::💡 Sympathetic ganglion of C7–T1 near the first rib supplying head, neck and upper limb))
- ((Ciliary::Parasympathetic ganglion for CN III to eye muscles))
Damage to which of the following causes Horner’s syndrome in a patient with a Pancoast tumour?
- ((Posterior root of sympathetic::Carries postganglionic fibres))
- ((Lateral root of sympathetic::💡 Preganglionic fibres from intermediolateral cell column at T1))
- ((Anterior root of sympathetic::Contains postganglionic fibres to targets))
- ((Edinger–Westphal nucleus::Parasympathetic pupil constriction))
A patient undergoes right thoracoscopic sympathectomy for axillary hyperhidrosis. Diathermy injury may result in:
- ((Hoarseness::Recurrent laryngeal nerve injury))
- ((Horner’s syndrome::💡 Damage to stellate ganglion sympathetic fibres))
- ((Raised right hemidiaphragm::Phrenic nerve injury))
- ((Reduced biceps tendon reflex::Not related))
A 55-year-old has spastic paralysis and an extensor plantar reflex. Where is the lesion?
- ((Posterior (dorsal) horn of spinal cord::Sensory processing region))
- ((Cerebellum::Coordinates movement))
- ((Basal ganglia::Movement modulation))
- ((Anterior horn of spinal cord::Lower motor neurones))
- ((None of the above::💡 Spasticity, hypertonia, hyperreflexia and extensor plantar indicate UMN damage))
A patient has intrinsic hand muscles’ weakness and loss of sensation over the inner aspect of the arm. Diagnosis?
- ((Thoracic outlet syndrome::Compression at scalene region))
- ((Superior sulcus tumour::💡 Pancoast tumour affecting lower plexus → intrinsic hand weakness + medial arm sensory loss))
- ((Carpal tunnel syndrome::Median nerve compression))
- ((Cubital tunnel syndrome::Ulnar nerve entrapment))
A Pancoast (superior sulcus) tumor compresses the lower brachial plexus C8 and T1, causing both intrinsic hand weakness and medial arm sensory loss.
Gate Control Theory of Pain
TENS is based on the "Gate Control Theory" of pain: TENS stimulates Aβ touch/pressure fibres, which inhibits transmission of pain via the Aδ and C fibres. This reduces pain signalling to the brain, so pain feels less intense.
Slow transmission of mechanothermal stimuli is transmitted via C fibres. Aγ fibres transmit motor proprioception information, Aβ fibres transmit touch and pressure and B fibres are autonomic fibres.
How does transcutaneous electrical nerve stimulation (TENS) relieve chronic pain?
- ((Inhibition of posterior horn of grey matter::💡 Gate control theory reducing nociceptive transmission))
- ((Inhibition of reticular activating system::Wakefulness modulation))
- ((Inhibition of Na⁺ channel activity::Local anaesthetic mechanism))
- ((Release of substance P::Promotes pain transmission))
A patient’s abdominal pain is relieved by rubbing and applying a warm cloth. The pain relief mechanism is due to which neural interaction?
- ((C fibre modulation by A-beta fibres::💡 Gate control theory where large-diameter mechanoreceptor fibres inhibit nociceptive transmission))
- ((A-delta fibre facilitation by C fibres::Fast pain pathway enhancement))
- ((Sympathetic fibre inhibition of nociceptors::Autonomic modulation))
- ((Spinothalamic tract activation::Ascending pain transmission))
According to the gate control theory, A-beta fibres (touch/pressure) stimulate inhibitory interneurons in the spinal cord, which suppress transmission from C-fibres (slow pain) leading to pain relief by rubbing, massage, or warmth.
Anterior cord syndrome
Anterior cord syndrome describes damage to the anterior ⅔ of the spinal cord, affecting corticospinal and spinothalamic tracts but preserving dorsal column function. Anterior cord syndrome results in:
- Bilateral flaccid paralysis at the level
- At the level, LMN anterior horn cells are destroyed: Flaccid weakness and areflexia at that level
- UMN signs including spasticity below
- Below the injury, the muscles are still connected to their LMNs, but the brain can’t control them: UMN signs including spastic weakness, hyperreflexia, and Babinski sign
- Bilateral loss of pain and temperature sensation below the lesion.
- Vibration and proprioception are spared
A man has back pain and lower-limb weakness due to a central disc prolapse causing LMN signs. Diagnosis?
- ((Central cord syndrome::Upper limb weakness and cape-like pain and temperature loss))
- ((Brown-Séquard syndrome::Ipsilateral motor and proprioceptive loss with contralateral pain and temperature loss))
- ((Posterior cord syndrome::Proprioceptive loss below lesion))
- ((Anterior cord syndrome::💡 Bilateral flaccid paralysis at level with spasticity and pain/temperature loss below))
Cauda equina syndrome
Cauda equina syndrome describes compression of cord below L1/L2 causing bilateral LMN signs of paralysis and reduced reflexes, sensory loss in a saddle distribution, and bladder, bowel and sexual dysfunction. Immediate MRI and surgical decompression usually within 24-48 hours are required.
A patient presents with urine retention and features of cauda equina syndrome. Which would not be expected?
- ((Urine retention::Common due to bladder dysfunction))
- ((Knee hyperreflexia::💡 Cauda equina causes LMN signs with hypo- or areflexia))
- ((Overflow incontinence::Occurs from chronic retention))
- ((Saddle anaesthesia::Perineal sensory loss from sacral root involvement))
Brown-Séquard syndrome
Brown-Séquard syndrome, hemisection of one cord side which affects the:
- Corticospinal tract → Ipsilateral weakness
- Dorsal column → Ipsilateral loss of proprioception, vibration, fine touch
- Spinothalamic tract → Contralateral loss of pain and temperature
Which of the following describes the features of Brown–Séquard syndrome following a spinal cord hemisection?
- ((Ipsilateral weakness and contralateral loss of temperature distally::💡 Hemisection causes ipsilateral corticospinal loss with contralateral spinothalamic loss))
- ((Bilateral weakness and bilateral loss of sensation::Complete cord transection))
- ((Isolated lower motor neurone weakness::Anterior horn or peripheral nerve lesion))
- ((Sensory level without motor involvement::Posterior cord syndrome))
A woman sustains a gunshot transecting her spinal cord on the left. Which picture fits Brown–Séquard syndrome?
- ((Ipsilateral weakness, ipsilateral loss of proprioception & vibration, contralateral loss of pain & temperature::💡 Classic hemisection pattern))
- ((Contralateral weakness, ipsilateral proprioception loss, contralateral pain & temperature loss::Ipsilateral weakness, ipsilateral loss of proprioception & vibration, contralateral loss of pain & temperature))
- ((Ipsilateral weakness, contralateral proprioception & vibration loss, contralateral pain & temperature loss::Ipsilateral weakness, ipsilateral loss of proprioception & vibration, contralateral loss of pain & temperature))
- ((Ipsilateral weakness, contralateral proprioception loss, ipsilateral pain & temperature loss::Ipsilateral weakness, ipsilateral loss of proprioception & vibration, contralateral loss of pain & temperature))
Syringomyelia
Syringomyelia produces a “cape‑like” loss of pain and temperature as syrinx expansion in the central cord interrupts the crossing of spinothalamic fibres in the anterior commissure.
An elderly man with an Arnold–Chiari malformation develops syringomyelia. Which of the following fibre tracts is most likely disrupted?
- ((Lesion in spinothalamic tract::💡 Central cord cavitation interrupts decussating pain and temperature fibres))
- ((Meningocele::CSF sac only with no neural tissue involvement))
- ((Meningomyelocele::Protrusion of cord elements, not specific to syrinx formation))
- ((Hydrocephalus::May accompany Chiari but not the direct cause of syrinx))
- ((Syringobulbia::Extension into brainstem rather than initial spinal cord lesion))
A 2-year-old child with Arnold–Chiari malformation develops syringomyelia. Which spinal tract is first affected?
- ((Spinothalamic tract::💡 Decussating pain and temperature fibres in the central cord are damaged first))
- ((Dorsal columns::Carry vibration and proprioception))
- ((Corticospinal tract::Motor pathways))
- ((Spinocerebellar tract::Unconscious proprioception))
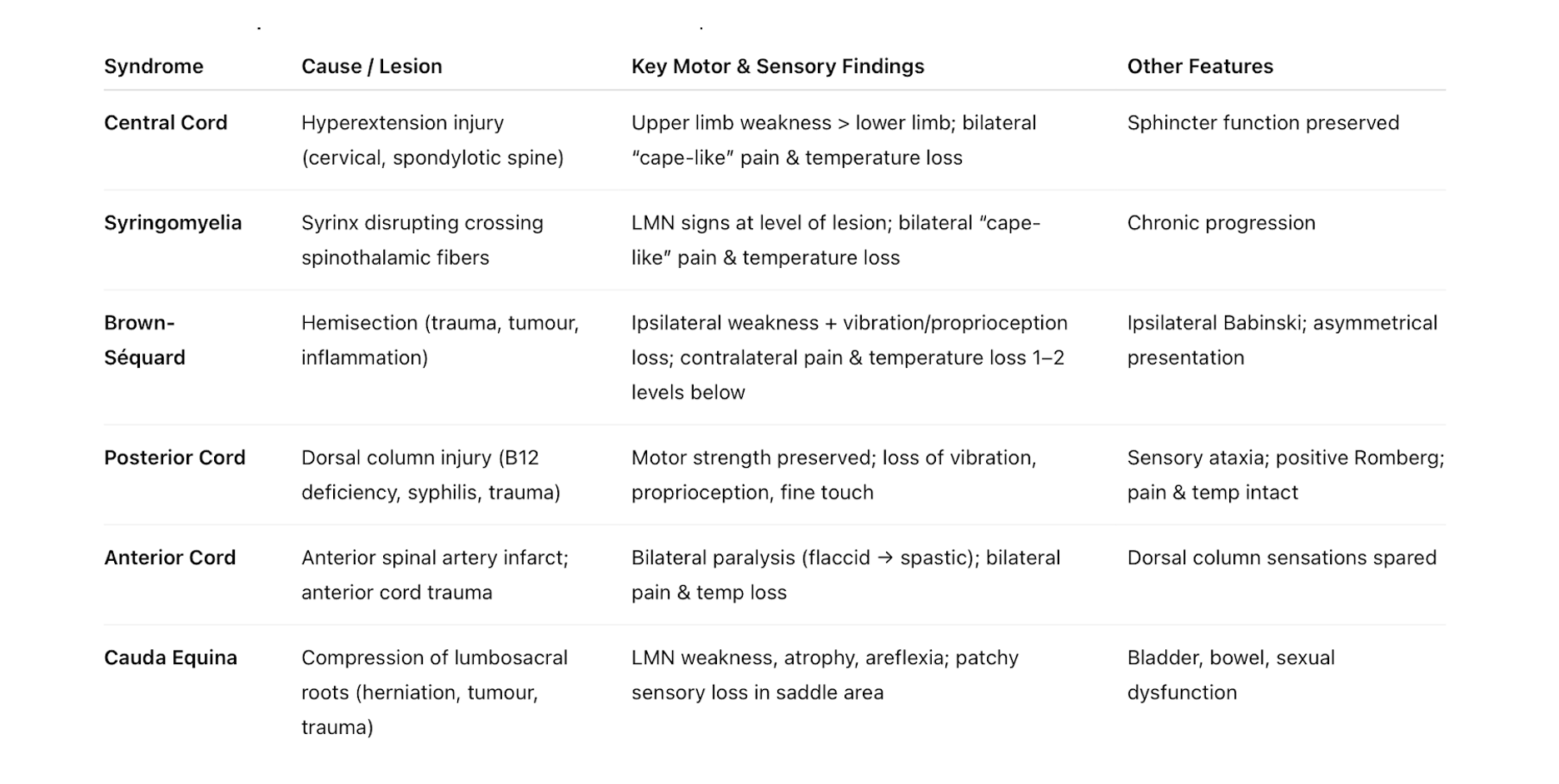
Spinal Cord Syndromes - Summary Table
👩⚕️ This is a summary table of the spinal cord syndrome that often appear in exams and their characteristic findings. Make sure you've memorised this!