Trigeminal CN V
Function
- First and foremost - remember that the trigeminal CN V's main function is providing sensation to the face.
- The trigeminal CN V only provides motor fibres through its mandibular division V3, supplying the muscles of mastication (masseter, temporalis, medial pterygoid and lateral pterygoid) as well as the mylohyoid, anterior belly of the digastric, tensor tympani and tensor veli palatini muscles. The rest of the face's motor function is mainly via the facial CN VII.
- Although the trigeminal CN V has no parasympathetic fibres of its own, its branches act as pathways carrying parasympathetic secretomotor fibres to the lacrimal, parotid, submandibular and sublingual glands via the pterygopalatine, otic, submandibular and ciliary ganglia. This will come up again in two lesson's time, don't worry.
It's not enough to know the trigeminal nerve provides sensation to the face. You need to know which branch of the trigeminal nerve provides sensation to different areas of the face....
Branches
The trigeminal CN V has three divisions (the ophthalmic V1, maxillary V2, and mandibular V3) but you need to know the branches of each division.
- The ophthalmic nerve of the trigeminal, CN V1, splits into x3 main branches -
- ((Lacrimal nerve::✨ Sensory: Lacrimal gland, upper eyelid, conjunctiva. 🌟 Parasympathetic: Carries post-ganglionic parasympathetic secretor motor fibres it receives from the zygomatic branch of maxillary V₂, to the lacrimal gland.))
- ((Frontal nerve::✨ Sensory: The frontal nerve divides into the supraorbital and supratrochlear nerves to supply sensation to the forehead, scalp up to the vertex, upper eyelid, medial forehead, and part of the nasal bridge.))
- ((Supraorbital::✨ Sensory: The supraorbital nerve is a branch of the frontal nerve which supplies sensation to the forehead, scalp up to the vertex, upper eyelid and the frontal sinus. Note that the infraorbital nerve is a branch of CN V2.))
- ((Supratrochlear::✨ Sensory: The supratrochlear nerve is a branch of the frontal nerve which supplies sensation to the medial forehead, medial upper eyelid and upper nasal bridge. Note that the infratrochlear nerve branches off the CN V1's nasociliary nerve.))
- ((Nasociliary nerve::✨ Sensory: The nasociliary nerve forms the afferent limb of the corneal reflex and its branches provide sensation to the cornea, dorsum and tip of the nose, parts of the nasal cavity, nasal mucosa and ethmoidal air cells, medial canthus, upper nasal bridge and it forms the afferent limb of the corneal reflex.))
- Long ciliary nerves
- Short ciliary nerves (via ciliary ganglion)
- Infratrochlear
- Anterior ethmoidal
- External nasal branch
- Internal nasal branches
- Posterior ethmoidal
- The maxillary nerve of the trigeminal, CN V2, purely sensory, passes through the foramen rotundum into the pterygopalatine fossa, where it gives off the:
- ((Zygomatic nerve::✨ Sensory: The zygomatic nerve divides into the zygomaticofacial and zygomaticotemporal nerves, supplying sensation to the cheek prominence and temple.))
- Zygomaticofacial
- Zygomaticotemporal
- ((Infraorbital nerve::✨ Sensory: The infraorbital nerve continues through the infraorbital canal, giving off the anterior and middle superior alveolar nerves to the upper incisors, canines and premolars, and emerges onto the face to supply the lower eyelid, upper lip, and lateral nose.))
- Anterior superior alveolar
- Middle superior alveolar
- Inferior palpebral
- External nasal
- Superior labial
- ((Zygomatic nerve::✨ Sensory: The zygomatic nerve divides into the zygomaticofacial and zygomaticotemporal nerves, supplying sensation to the cheek prominence and temple.))
- ((Posterior superior alveolar nerve::✨ Sensory: Maxillary molar teeth and adjacent buccal gingiva.))
- ((Greater palatine nerve::✨ Sensory: Hard palate, palatal gingiva of the maxillary molars and premolars.))
- ((Lesser palatine nerve::✨ Sensory: Soft palate, uvula, and tonsillar region.))
- ((Nasopalatine nerve::✨ Sensory: Nasal septum and the anterior hard palate behind the upper incisors.))
- ((Pharyngeal branch::✨ Sensory: The pharyngeal branch (of the pterygopalatine ganglion) supplies sensation to the nasopharynx.))
- ((Meningeal branch (middle meningeal nerve)::✨ Sensory: Dura mater of the anterior aspect of the middle cranial fossa.))
- The mandibular nerve of the trigeminal, CN V₃, is the only mixed division carrying both sensory and motor fibres; it passes through the foramen ovale into the infratemporal fossa, where it immediately divides into its sensory and motor branches. The sensory and motor branches are listed separately below -
Sensory branches:
- ((Auriculotemporal nerve::✨ Sensory: Temple, auricle, external acoustic meatus and temporomandibular joint. 🌟 Parasympathetic: It also carries parasympathetic fibres to the parotid gland.))
- ((Buccal nerve::✨ Sensory: Buccal mucosa, molar teeth, gingiva.))
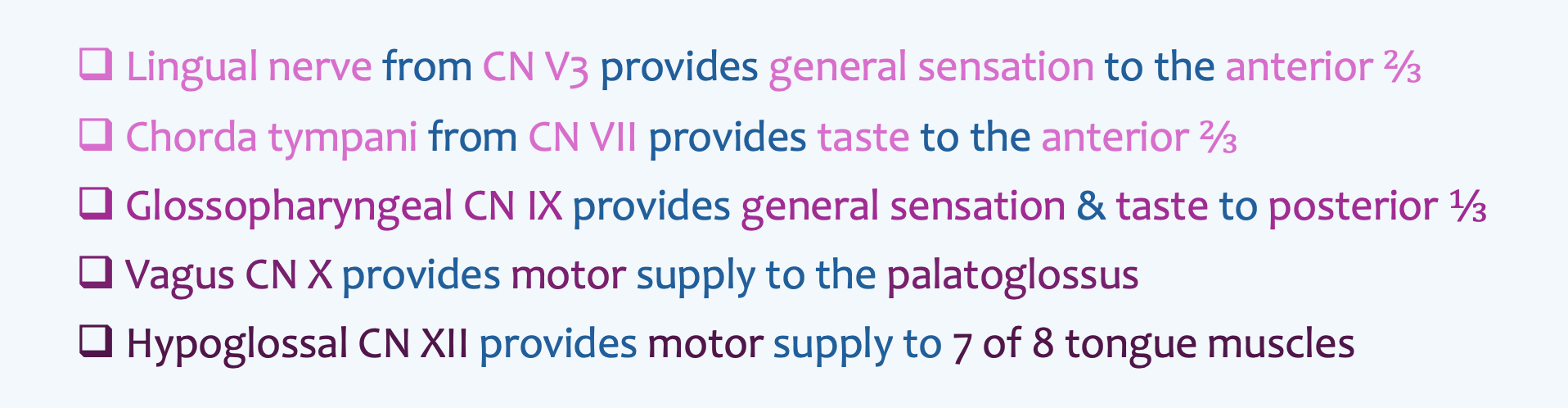
- ((Lingual nerve::✨ Sensory: General sensation to the anterior 2/3 of the tongue, floor of the mouth, and lingual gingiva. 🌟 Parasympathetic: It later receives the chorda tympani from facial CN VII, which adds taste fibres for the anterior tongue and parasympathetic secretomotor fibres to the submandibular and sublingual glands via the submandibular ganglion.))
- ((Inferior alveolar nerve::✨ Sensory: Lower teeth and, via the mental nerve, the lower lip and chin.))
- ((Mental nerve::The mental nerve is a terminal branch of the inferior alveolar n., is a branch of the trigeminal’s mandibular CN V3. ✨ Sensory: The mental nerve exits the mental foramen to supply the skin of the lower lip, gingiva and chin. It is vulnerable in dental surgery. Injury to the mental nerve would present as numbness of the lower lip and chin.))
- Incisive branch
- ((Meningeal branch (nervus spinosus)::Re-enters the skull through the foramen spinosum alongside the middle meningeal artery. ✨ Sensory: Dura mater of the majority of the middle cranial fossa.))
Motor branches:
- ((Deep temporal nerves::✨ Motor: Temporalis muscle.))
- ((Masseteric nerve::✨ Motor: Masseter muscle. ))
- ((Medial pterygoid nerve::✨ Motor: Medial pterygoid muscle and also gives branches to the tensor veli palatini and tensor tympani muscles.))
- ((Branch to tensor veli palatini::The tensor veli palatini tenses the soft palate and opens the pharyngotympanic (Eustachian) tube during swallowing and yawning, helping equalise pressure between the nasopharynx and middle ear.))
- ((Branch to tensor tympani::The tensor tympani dampens loud sounds by pulling the handle of the malleus medially and tensing the tympanic membrane, reducing the amplitude of vibrations reaching the inner ear.))
- ((Lateral pterygoid nerve::✨ Motor: Lateral pterygoid muscle.))
- ((Nerve to mylohyoid::✨ Motor: Mylohyoid muscle and the anterior belly of the digastric.)
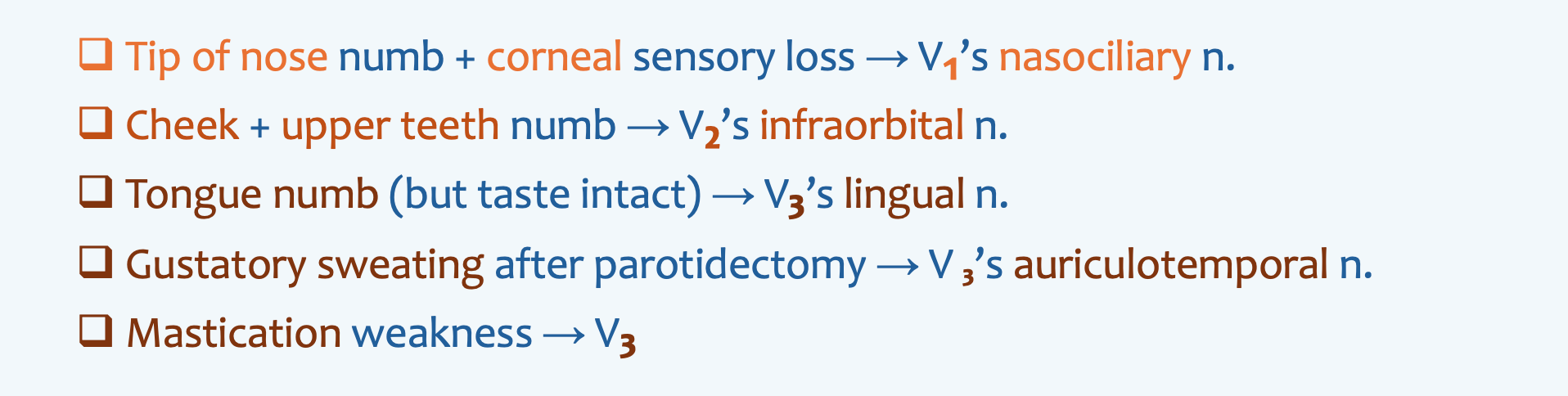
Very high-yield Trigeminal CN V 1-3 patterns
Innervation to the tongue
A 22‑year‑old woman has lost sensation over the tip of her nose. Where else is sensation likely to be lost?
- ((Hard palate::The CN V2's greater palatine nerve provides sensation to the hard palate))
- ((Soft palate::The CN V2's lesser palatine branch and CN IX provide sensation to the soft palate))
- ((Ear pinna::Supplied by multiple nerves including greater auricular, lesser occipital and auriculotemporal nerves))
- [[Cornea::Branches of CN V1's nasociliary nerve include the external nasal nerve (CN V1 > nasociliary nerve > anterior ethmoidal nerve > external nasal nerve), which supplies the nasal tip, and the long ciliary nerves (CN V1 > nasociliary nerve > short/long ciliary nerves) which provides sensation from the cornea.
A patient presents with numbness of the cheek, upper frontal teeth, and anesthesia of the lateral side of the nose following facial trauma. Which nerve is most likely injured?
- [[Infraorbital::This terminal branch of maxillary CN V₂ is classically injured in orbital floor and zygomatic fractures. Injury to the infraorbital nerve causes numbness of the lower eyelid, upper lip, lateral nose and upper anterior teeth, often described as loss of sensation over the cheek and upper gum following midface or orbital floor trauma.]]
- ((Infratrochlear::Infratrochlear nerve branches off the CN V1's nasociliary nerve and supplies the medial canthus and bridge of the nose.))
- ((Supratrochlear::Supratrochlear nerve branches of the CN V1's frontal nerve and supplies the medial forehead and upper eyelid.))
- ((Anterior superior alveolar::The anterior superior alveolar nerve is a branch of the infraorbital nerve, itself a terminal branch of maxillary CN V₂; it supplies the upper incisors.))
The infraorbital nerve, the terminal branch of the trigeminal’s maxillary CN V2, exits via the infraorbital foramen. Within the infraorbital canal, the infraorbital nerve gives off the middle and anterior superior alveolar nerves. Emerging from the infraorbital canal, it gives off the inferior palpebral, nasal and superior labral branches.
It may be injured in zygomatic or orbital floor fractures, causing numbness of the lower eyelid, cheek, lateral nose, upper lip, upper incisors and canines.
A 21-year-old man undergoes surgical removal of an impacted third molar. Post-operatively, he has anaesthesia of the anterolateral tongue. What nerve was most likely injured?
- ((Marginal mandibular branch::Marginal mandibular branch is a motor branch of the facial CN VII nerve))
- ((Hypoglossal CN XII::The hypoglossal CN XII provides motor innervation to 7 of 8 tongue muscles))
- ((Glossopharyngeal CN IX::The glossopharyngeal CN IX provides general and taste sensation from posterior ⅓ of tongue, and sensation from the middle ear))
- ((Inferior alveolar nerve: The inferior alveolar nerve from CN V3 provides sensation from lower teeth, lower gum, lower lip and chin))
- [[Lingual::The lingual nerve from CN V3 provides general sensation to the anterior ⅔ of the tongue. ]]
A 23-year-old woman with sialolithiasis of the submandibular gland is undergoing surgical excision. During mobilisation of the submandibular duct, which nerve is most at risk?
- ((Hypoglossal CN XII::Motor supply to tongue muscles, not closely related to the submandibular duct))
- ((Marginal mandibular branch::Superficial facial CN VII branch supplying lower lip muscles))
- ((Inferior alveolar nerve::Runs within the mandibular canal supplying sensation to the lower teeth))
- [[Lingual::The lingual nerve is medial to the 3rd molar and near to the submandibular duct, so it’s highly vulnerable during lower 3rd molar extraction and submandibular duct mobilisation or removal.]]
- ((Glossopharyngeal CN IX::Supplies posterior tongue sensation; not involved in submandibular duct surgery))
During a parotidectomy, transection of the facial nerve is a risk. Which would not result from facial nerve injury?
- [[Numbness over the cheek::Sensation to the face is mostly provided by the trigeminal CN V branches, not the facial CN VII]]
- ((Loss of corneal reflex::The efferent pathway of the corneal reflex is the facial CN VII, which carries motor signals from the brainstem to the orbicularis oculi muscle to cause blinking))
- ((Lower lip dropping::Depressor labii inferioris is supplied by the marginal mandibular branch of the facial CN VII))
- ((Drop angle of mouth::Depressor anguli oris is supplied by buccal and marginal mandibular branch of the facial CN VII))
A patient develops gustatory sweating following a parotidectomy. What is the mechanism behind this condition?
- [[Regeneration of parasympathetic fibres of the auriculotemporal nerve innervating the sweat gland::Frey’s syndrome is the misguided regrowth of parasympathetic fibres into sweat glands causes sweating when eating]]
- ((Regeneration of sympathetic fibres onto the parasympathetic fibres of the auriculotemporal nerve::It is the parasympathetic, not sympathetic nerves, regrow along the wrong pathway into the sweat glands and blood vessels of the skin instead of growing to the parotid gland))
- ((Regeneration of facial nerve after its injury::Would cause facial weakness, not gustatory sweating))
- ((Regeneration of great auricular nerve onto sympathetic fibres innervating sweat glands::Great auricular nerve does not carry parasympathetic fibres))
The auriculotemporal nerve is a branch of the mandibular CN V3, which has three functions:
- Sensory from the temple, TMJ, external acoustic meatus, anterior to auricle, tragus, crus
- Receives post-ganglionic (otic ganglion) parasympathetic fibres from the lesser petrosal nerve to the parotid gland for saliva production
- Inferior salivatory nucleus → Glossopharyngeal CN IX → Tympanic n. of Jacobson → Passes through the jugular foramen and enters the middle ear to form the tympanic plexus → Lesser petrosal n. → Exit the skull through the foramen ovale → Otic ganglion → Joins the auriculotemporal branch of V3 → Parotid gland
- Sympathetic fibres to the sweat glands and blood vessels of the skin
Frey’s syndrome (gustatory sweating) happens when the auriculotemporal nerve is damaged e.g. during parotid surgery. As the nerve heals, the parasympathetic fibres regrow along the wrong pathway into the sweat glands and blood vessels of the skin instead of growing to the parotid gland. As a result, when the patient eats and the body tries to stimulate salivation, it instead triggers sweating and flushing over the area near the parotid.
The middle meningeal artery is closely related to the auriculotemporal nerve; the nerve actually wraps around the artery, making both structures easy to identify in anatomy dissections but also vulnerable during surgery.
A patient suffers an orbital floor fracture and now has loss of lacrimation. Which nerve is most likely affected?
- ((Lacrimal nerve::Carries sensory fibres plus parasympathetic fibres from CN VII, but only as a conduit; an isolated lacrimal nerve injury is less likely to abolish lacrimation))
- ((Facial nerve::Would cause widespread facial paralysis, not isolated loss of lacrimation))
- [[Greater petrosal nerve::Provides the parasympathetic fibres that stimulate lacrimal gland secretion; disruption results in loss of lacrimation]]
- ((Auriculotemporal nerve::Carries parasympathetic fibres to the parotid gland, unrelated to lacrimal secretion))
Lacrimation reflex pathway: Conjunctiva irritation → Lacrimal n. → Ophthalmic n. (V1) → Trigeminal sensory centre → Superior salivary nucleus → Facial CN VII → Greater petrosal n. → Pterygopalatine ganglion → Joins zygomatic branch of trigeminal’s maxillary CN V2 → Joins the lacrimal branch of V1 → Lacrimal apparatus
Arterial supply to the lacrimal system is via a lacrimal branch of the ophthalmic artery from the internal carotid artery.
Venous drainage is to the superior ophthalmic vein.